Cervical cancer
The cervix is the lower, narrow end of the uterus (the hollow, pear-shaped organ where a fetus grows). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through a series of changes in which cells that are not normal begin to appear in the cervical tissue. When cells change from being normal cells to abnormal cells, it is called dysplasia. Depending on the number of abnormal cells, dysplasia may go away without treatment. The more abnormal cells there are, the less likely they are to go away. Dysplasia that is not treated may turn into cancer, over time. The cancer cells grow and spread through the cervix. It can take many years for dysplasia to turn into cancer
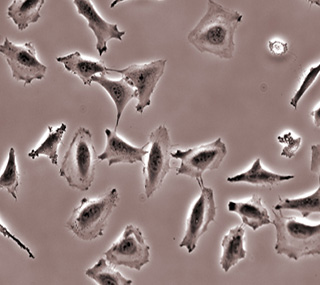
Cervical cancer may not have symptoms but can be found with regular Pap tests (a procedure in which cells are scraped from the cervix and looked at under a microscope). Cervical cancer is almost always caused by human papillomavirus (HPV) infection.
UC Davis Comprehensive Cancer Center provides comprehensive, multidisciplinary care for patients with cervical cancer. Patients receive all of their care from a team of top academic physicians.
 Regular pelvic exams and Pap tests help find abnormal cells in the cervix before cancer develops. However, test and procedures that may be used after an abnormal pelvic exam or Pap test result have risks. For example, the treatment of low-grade lesions may affect a woman's ability to become pregnant or carry a baby to full term. In women younger than 25 years, screening with the Pap test has more risks than benefits. Screening with the Pap test is not helpful in women older than 60 years who have had recent negative Pap tests.
Regular pelvic exams and Pap tests help find abnormal cells in the cervix before cancer develops. However, test and procedures that may be used after an abnormal pelvic exam or Pap test result have risks. For example, the treatment of low-grade lesions may affect a woman's ability to become pregnant or carry a baby to full term. In women younger than 25 years, screening with the Pap test has more risks than benefits. Screening with the Pap test is not helpful in women older than 60 years who have had recent negative Pap tests.
Sources: National Cancer Institute and UC Davis Comprehensive Cancer Center
There are usually no noticeable signs of early cervical cancer but it can be detected early with yearly check-ups, including a Pap smear to check for abnormal cells in the cervix. The prognosis (chance of recovery) is better when the cancer is found early.
Possible signs of cervical cancer include vaginal bleeding and pelvic pain, but other conditions may cause the same symptoms. A doctor should be consulted if any of the following problems occur:
Sources: National Cancer Institute and UC Davis Comprehensive Cancer Center
HPV Infection
The most common cause of cervical cancer is infection of the cervix with human papillomavirus (HPV). There are more than 80 types of human papillomavirus. About 30 types can infect the cervix and about half of them have been linked to cervical cancer. HPV infection is common but only a very small number of women infected with HPV develop cervical cancer.
HPV infections that cause cervical cancer are spread mainly through sexual contact. Women who become sexually active at a young age and who have many sexual partners are at a greater risk of HPV infection and developing cervical cancer.
Smoking
Smoking cigarettes and breathing in secondhand smoke increase the risk of cervical cancer. Among women infected with HPV, dysplasia and invasive cancer occur 2 to 3 times more often in current and former smokers. Secondhand smoke causes a smaller increase in risk.
The following risk factors may increase the risk of cervical cancer:
High number of full-term pregnancies
Women who have had 7 or more full-term pregnancies may have an increased risk of cervical cancer.
Long-term use of oral contraceptives
Women who have used oral contraceptives ("the Pill") for 5 years or more have a greater risk of cervical cancer than women who have never used oral contraceptives. The risk is higher after 10 years of use.
Sources: National Cancer Institute and UC Davis Comprehensive Cancer Center
Surgery
Surgery (removing the cancer in an operation) is sometimes used to treat cervical cancer. The following surgical procedures may be used:
- Conization: A procedure to remove a cone-shaped piece of tissue from the cervix and cervical canal. A pathologist views the tissue under a microscope to look for cancer cells. Conization may be used to diagnose or treat a cervical condition. This procedure is also called a cone biopsy.
- Total hysterectomy: Surgery to remove the uterus, including the cervix. If the uterus and cervix are taken out through the vagina, the operation is called a vaginal hysterectomy. If the uterus and cervix are taken out through a large incision (cut) in the abdomen, the operation is called a total abdominal hysterectomy. If the uterus and cervix are taken out through a small incision in the abdomen using a laparoscope, the operation is called a total laparoscopic hysterectomy.
- Radical hysterectomy: Surgery to remove the uterus, cervix, part of the vagina, and a wide area of ligaments and tissues around these organs. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
- Modified radical hysterectomy: Surgery to remove the uterus, cervix, upper part of the vagina, and ligaments and tissues that closely surround these organs. Nearby lymph nodes may also be removed. In this type of surgery, not as many tissues and/or organs are removed as in a radical hysterectomy.
- Bilateral salpingo-oophorectomy: Surgery to remove both ovaries and both fallopian tubes.
- Pelvic exenteration: Surgery to remove the lower colon, rectum, and bladder. In women, the cervix, vagina, ovaries, and nearby lymph nodes are also removed. Artificial openings (stoma) are made for urine and stool to flow from the body to a collection bag. Plastic surgery may be needed to make an artificial vagina after this operation.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue, such as carcinoma in situ. This type of treatment is also called cryotherapy.
- Laser surgery: A surgical procedure that uses a laser beam (a narrow beam of intense light) as a knife to make bloodless cuts in tissue or to remove a surface lesion such as a tumor.
- Loop electrosurgical excision procedure (LEEP): A treatment that uses electrical current passed through a thin wire loop as a knife to remove abnormal tissue or cancer.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy. External radiation therapy uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer. The way the radiation therapy is given depends on the type and stage of the cancer being treated.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the spinal column, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
The close collaboration among our doctors and our research scientists means that new drugs and treatments developed in the laboratory can quickly move to the clinic, offering our patients immediate access to the latest therapies.
Clinical Trials
UC Davis Comprehensive Cancer Center has a large clinical trials network. We are an affiliate member of the Gynecology Oncology Group, offering our patients access to the newest drugs and therapies before they become widely available. During all stages of your treatment you should talk to your medical specialist about what clinical trials may be available for you.
Sources: National Cancer Institute and UC Davis Comprehensive Cancer Center
Gynecologic Oncology (Surgery)
 Rebecca Ann Brooks, M.D.
Rebecca Ann Brooks, M.D.
Associate Professor, Gynecologic Oncology
 Hui (Amy) Chen, M.D.
Hui (Amy) Chen, M.D.
Assistant Clinical Professor, Gynecologic Oncology
 Gary S. Leiserowitz, M.D.
Gary S. Leiserowitz, M.D.
Professor and Chief, Gynecologic Oncology
Fellowship Director, Gynecologic Oncology
 Rachel Ruskin, M.D.
Rachel Ruskin, M.D.
Assistant Professor, Gynecologic Oncology
Radiation Oncology
 Richard Valicenti, M.D., M.A., FASTRO
Richard Valicenti, M.D., M.A., FASTRO
Professor
Department Chair of Radiation Oncology
Dietitians
 Danielle Baham, M.S., R.D.
Danielle Baham, M.S., R.D.
 Kathleen Newman, R.D., C.S.O.
Kathleen Newman, R.D., C.S.O.
Genetic Counselors
Social Workers
 Sara Chavez, L.C.S.W., O.S.W.-C., A.C.H.P.-S.W.
Sara Chavez, L.C.S.W., O.S.W.-C., A.C.H.P.-S.W.
 Jenifer Cooreman, L.C.S.W., O.S.W.-C.
Jenifer Cooreman, L.C.S.W., O.S.W.-C.





 Nicole Mans, M.S., L.C.G.C.
Nicole Mans, M.S., L.C.G.C. Jeanna Welborn, M.D.
Jeanna Welborn, M.D.