Resident Research Projects

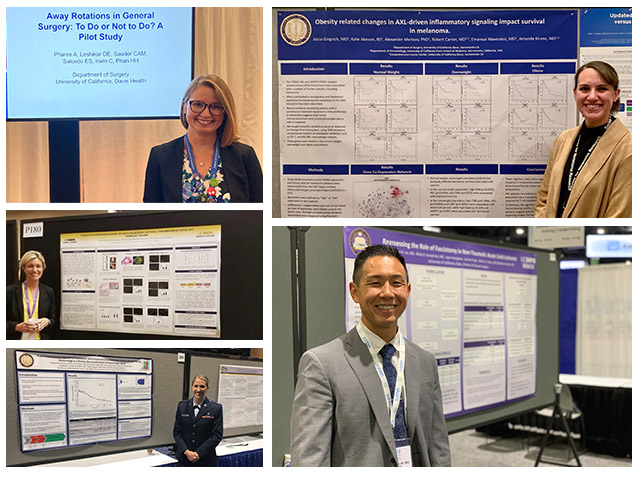
The Burn Surgery division is extremely active in both clinical and basic science research projects. Some of the ongoing clinical topics include frailty, age and TBSA as predictors of morbidity and mortality, the use of biodegradable temporizing matrix for coverage of burn excision sites, the impact of wildfires on burn center admissions and patient outcomes, and the identification of acute kidney injury and sepsis using artificial intelligence. The basic science research lab is focused on mutations in the human glucocorticoid receptor in response to damage and pathogen associated molecular patterns. Residents have had the opportunity to participate in each of these project areas either during their clinical years or during dedicated research time, and have presented their results at national meetings
Research in the Colorectal department focuses a diverse breadth of clinical outcomes and initiatives. Among these are studies focused on refining the management of diverticulitis (including participation in multi-institutional trials), predictors of readmission in patients undergoing ileostomy creation, disparities in rectal cancer care and outcomes based on geography and race, and finally investigating the impact of robotic surgery on outcomes, cost, and value for general surgery and colorectal surgery indications. Our colorectal faculty have a passion for working with residents and a longstanding reputation as experienced mentors.
Multiple residents and faculty members at UC Davis have an interest in research in surgical education, simulation, and the learning environment. Recent projects include developing innovative curricula, designing simulators for procedural training, improving operative feedback, expanding robotic surgery training, investigating the impact of microaggressions on residency training, creating a peer support program, and assessing the needs of resident-parents. We also have the option for residents to complete the UC Davis Surgical Education Fellowship during the research years. (See Surgeon Educator: https://health.ucdavis.edu/surgery/education/training_tracks.html)
 There a number of ongoing research opportunities in the division of Pediatric Surgery. Residents often spend 1-2 years in the Surgical Bioengineering Laboratory with Dr. Farmer, studying augmentation of fetal myelomeningocele repair, in addition to numerous cell-based basic science projects, including diseases such as neuroblastoma and spinal cord injury. Many clinical projects are ongoing as well, including studies of pediatric trauma outcomes using our robust institutional trauma registry, and management and outcomes of many pediatric surgical diseases and treatments such as appendicitis, ECMO, Hirschsprung disease, pediatric surgical oncology, and many others. Residents frequently present their work at national conferences including the American Pediatric Surgical Association (APSA), the American Academy of Pediatrics (AAP), the Pacific Association of Pediatric Surgeons (PAPS), Pacific Coast Surgical Association (PCSA), Academic Surgical Congress (ASC), American College of Surgeons (ACS), Western Pediatric Trauma (WPT), and Pediatric Trauma Society (PTS). Additionally, residents have obtained Masters in Clinical and Translational Research during their time in the lab.
There a number of ongoing research opportunities in the division of Pediatric Surgery. Residents often spend 1-2 years in the Surgical Bioengineering Laboratory with Dr. Farmer, studying augmentation of fetal myelomeningocele repair, in addition to numerous cell-based basic science projects, including diseases such as neuroblastoma and spinal cord injury. Many clinical projects are ongoing as well, including studies of pediatric trauma outcomes using our robust institutional trauma registry, and management and outcomes of many pediatric surgical diseases and treatments such as appendicitis, ECMO, Hirschsprung disease, pediatric surgical oncology, and many others. Residents frequently present their work at national conferences including the American Pediatric Surgical Association (APSA), the American Academy of Pediatrics (AAP), the Pacific Association of Pediatric Surgeons (PAPS), Pacific Coast Surgical Association (PCSA), Academic Surgical Congress (ASC), American College of Surgeons (ACS), Western Pediatric Trauma (WPT), and Pediatric Trauma Society (PTS). Additionally, residents have obtained Masters in Clinical and Translational Research during their time in the lab.
 Research in the Division of Surgical Oncology is diverse, with ample opportunity for residents to become involved with basic science or clinical outcomes research alongside our faculty. Our faculty are NIH-funded researchers with extensive experience in the development and mentoring of trainees. A major focus of the division is multi-disciplinary "Team Science" projects, which bring together multiple areas of expertise to tackle the biggest questions in cancer care today. We collaborate regularly with basic science labs on the main UC Davis campus, as well as the Genome Center and School of Veterinary Medicine. There is an available T32 grant for those interested in participating in multi-disciplinary projects. Some examples of recent or ongoing studies include the investigation of immune therapies for the treatment of sarcoma and melanoma, DNA/RNA-sequencing studies analyzing the response to immune therapies in sarcoma, clinical trials in a canine model for treatment of osteosarcoma, cost-effectiveness analyses and value in pancreatic cancer care, survival analyses in male breast cancer, disparities in treatment for hepatocellular carcinoma, and basic and translational science research in melanoma with specific interest in mechanisms of evasive resistance, tumor microenvironment signaling and immune response. We have a dedicated focus on clinical outcomes research, which involves large regional or national databases such as California Cancer Registry and Office of Statewide Health Planning and Development database, SEER-Medicare, and the National Cancer Database. Residents have a robust history of presentations and posters at national and international cancer meetings. Options to obtain graduate degrees during research years are available.
Research in the Division of Surgical Oncology is diverse, with ample opportunity for residents to become involved with basic science or clinical outcomes research alongside our faculty. Our faculty are NIH-funded researchers with extensive experience in the development and mentoring of trainees. A major focus of the division is multi-disciplinary "Team Science" projects, which bring together multiple areas of expertise to tackle the biggest questions in cancer care today. We collaborate regularly with basic science labs on the main UC Davis campus, as well as the Genome Center and School of Veterinary Medicine. There is an available T32 grant for those interested in participating in multi-disciplinary projects. Some examples of recent or ongoing studies include the investigation of immune therapies for the treatment of sarcoma and melanoma, DNA/RNA-sequencing studies analyzing the response to immune therapies in sarcoma, clinical trials in a canine model for treatment of osteosarcoma, cost-effectiveness analyses and value in pancreatic cancer care, survival analyses in male breast cancer, disparities in treatment for hepatocellular carcinoma, and basic and translational science research in melanoma with specific interest in mechanisms of evasive resistance, tumor microenvironment signaling and immune response. We have a dedicated focus on clinical outcomes research, which involves large regional or national databases such as California Cancer Registry and Office of Statewide Health Planning and Development database, SEER-Medicare, and the National Cancer Database. Residents have a robust history of presentations and posters at national and international cancer meetings. Options to obtain graduate degrees during research years are available.
The division of Thoracic surgery focuses on clinical research in a variety of areas. Current projects include evaluation of how hospital and surgeon volumes affect outcomes after lung and esophageal surgery, the effects of frailty on postoperative outcomes, the impact of enhanced recovery protocols including liposomal bupivacaine intercostal nerve blockade on postoperative opioid reliance and patient reported outcome measures of pain, the effects of time since smoking cessation on pulmonary outcomes, markers of health-related quality of life after lung cancer surgery, utilization of a smoking quitline to improve smoking cessation and longterm abstinence in thoracic surgery patient populations, and comparison of robotic and video-assisted thoracoscopic surgery outcomes.
Research in the Transplant department focuses on pediatric en bloc kidney transplantation from very small (<10 kg) donation after circulatory death (versus brain death) donors, the study of an novel ex vivo renal normothermic perfusion system, combined ex vivo hypothermic and normothermic perfusion for assessment of high-risk deceased donor human kidneys for transplantation, and long term graft success from marginal donors. Residents have contributed to work in each of these areas and presented their results at national meetings.

Faculty of the Trauma, Critical Care and Acute Care Surgery Division, with the help of residents, participate in a wide breadth of research covering both clinical and basic science. The department strives to improve patient care through all aspects of an injured patient’s course.
In the prehospital setting, there is a cooperative effort with the regional Emergency Medical Services to improve prehospital care protocols. Within the inpatient setting, there are various studies focusing on improving patient pain control including use of Magnesium infusion, Exparel injections for rib fractures and creation of multimodal pain regimens to reduce use of opioids. For critically ill patients, improving extubation protocols to reduce ARDS, investigating the pathophysiology of trauma-induced coagulopathy and incorporating artificial intelligence into trauma protocols are underway. In conjugation with our Active Duty Air Force Surgeons, there is a focus on improving hemorrhage control interventions such as REBOA and the use of TXA on the battle field.
In the post-hospital setting, we are evaluating patient’s access to care and identifying barriers for follow-up. Additionally, members of the division have developed a strong social outreach program for patients that were victims of violent injury by focusing on how to reduce injury and criminal recidivism in the most vulnerable citizens.


 The Department of Surgery is committed to providing excellent research opportunities for their residents. Most residents dedicate 1-2 years between their clinical 3rd and 4th year to pursue their research interests or work on career development. This time is very flexible and can be spent doing anything from basic science research or clinical outcomes research to pursuing an advanced degree in another field. This time is funded by the program and residents are not expected to secure their own funding. The department established the Surgical Research Committee to help align residents with faculty currently involved in research and to provide research/career guidance and mentorship.
The Department of Surgery is committed to providing excellent research opportunities for their residents. Most residents dedicate 1-2 years between their clinical 3rd and 4th year to pursue their research interests or work on career development. This time is very flexible and can be spent doing anything from basic science research or clinical outcomes research to pursuing an advanced degree in another field. This time is funded by the program and residents are not expected to secure their own funding. The department established the Surgical Research Committee to help align residents with faculty currently involved in research and to provide research/career guidance and mentorship. 