Radiation Dose Reporting
CT Dose Reporting:
Starting on July 1, 2012, new California legislation requires that specific CT scanner dose metrics be included in the radiology report, for all patients undergoing diagnostic CT scans. These reporting requirements do not apply to CT scans used for purposes other than diagnosis[1]. Two specific dose metrics are required to be reported: the volume computed tomography dose index (CTDIvol) and the dose length product (DLP). This document is intended to help physicians, patients, and other interested parties to understand what these dose metrics mean.
What is CTDIvol ?
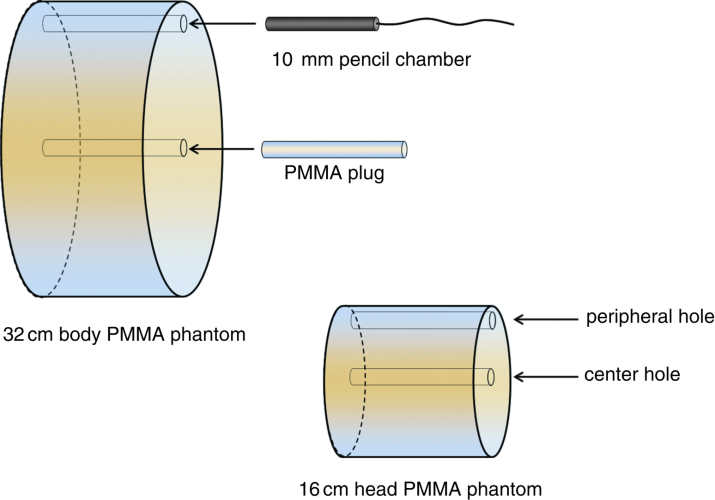
CTDIvol is a quantity that can be measured on either a large (32 cm diameter) or small (16 cm diameter) plastic cylinder (the type of plastic is called PMMA). Dose measurements are made at the center and at the periphery, and these values are combined using a weighted average to produce a single estimate of radiation dose to that plastic cylinder. The CTDIvol measured in the large phantom is used as a reference for adult CT in the torso (chest, abdomen, and pelvis) and also as a reference for pediatric body CT for some scanner manufacturers (Siemens, Philips). The CTDIvol measured in the small phantom is used as a reference for head CT, and also as a reference for pediatric body CT for some scanner manufacturers (General Electric, Toshiba, Hitachi). The CTDIvol value is reported in the units of mGy, where 10 mGy = 1 rad (an older unit of radiation dose). Once the CTDIvol values are measured on a particular CT scanner by the manufacturer, they are stored in a table and can be computed from the technique factors used to scan the patient.
The CTDIvol metric is a reasonable estimate of absorbed dose if the patient were comprised of plastic and if the patient had similar dimensions as the cylinder. If the patient size (effective diameter[2]) varies from the phantom diameter, adjustments to the indicated CTDIvol can be determined as described below. The phantom size used for the CTDIvol metric is indicated on the dose report for each acquisition event.
Large CTDI phantom: The 32 cm diameter phantom is about equivalent to somebody with a 47” waist line. In general, for body CT, most patients are smaller than the 32 cm diameter phantom, and this means that their actual dose from the scan will be higher than the CTDIvol value. The curve below provides an approximate correction factor, which can be a used to adjust the CTDIvol value for the size (effective diameter) of the patient.
Normalized CTDIvol Correction Factor: 32 cm diameter phantom
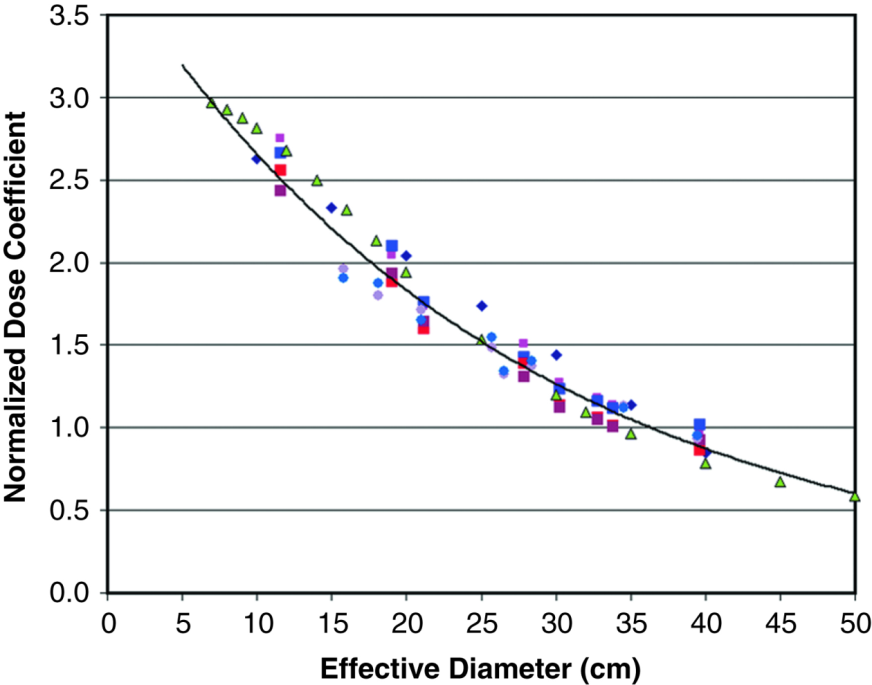
For patients who are larger than the body phantom, their actual dose values would be lower than the reported CTDIvol value. For most adult patients, the correction factors range from about +40% to -40%. For smaller pediatric patients (on Siemens and Philips scanners which use the 32 cm phantom), the reported CTDIvol underestimates the actual dose values in the range of 150% to 250%.
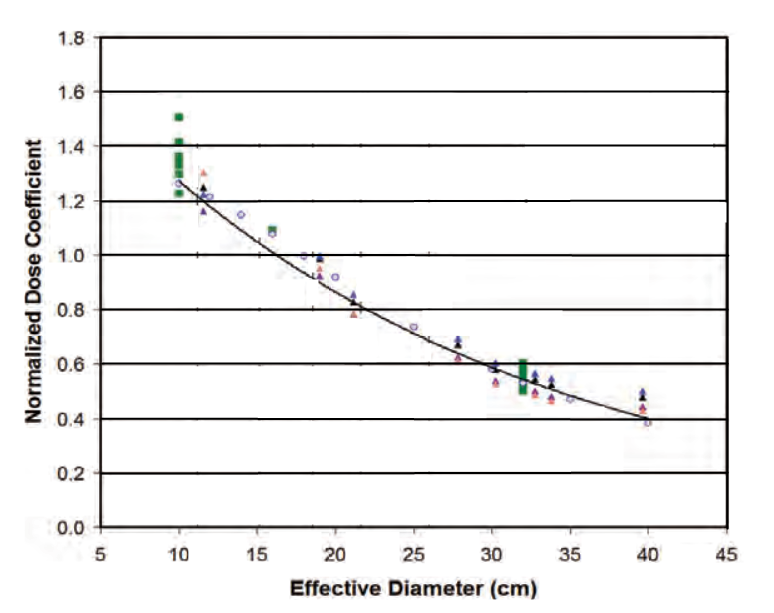
Small CTDI phantom: The 16 cm diameter phantom is used as a reference for head CT for all CT scanners and for pediatric body protocols for the General Electric, Toshiba, and Hitachi scanners. In general, most head scans match to the 16 cm diameter phantom reasonably well, and the correction factors to the reported CTDIvol are on the order of +20% to -20%. In the case of pediatric body scans, the reported CTDIvol value will overestimate the actual absorbed dose by 20% to 40% for larger pediatric patients with effective diameters of 20 cm to 30 cm.
Normalized CTDIvol Correction Factor: 16 cm diameter phantom
Absorbed dose is a measure of the x-ray energy absorbed per unit mass, and this ratio can sometimes be misleading. For example: compare a dose of 10 mGy to one finger (with a mass of about 10 grams) versus a dose of 1 mGy to the entire abdomen (a mass of about 25,000 grams). Clearly the lower dose to the torso involves a lot more x-ray energy being absorbed in the patient[3]. So in addition to dose, it is also useful to have an understanding of how much tissue was exposed. That is where DLP comes in...
What is DLP?
CT scans are performed over a length of the patient - sometimes they can be performed over a relatively short range in the patient, but more commonly they can extend greater distances, such as from the upper abdomen to the lower pelvis. The length of the scan is determined in centimeters (1 inch = 2.54 cm, 1 cm is about 3/8 inch), and the DLP is determined by multiplying the CTDIvol value by the scan length, resulting in the units of mGy-cm.
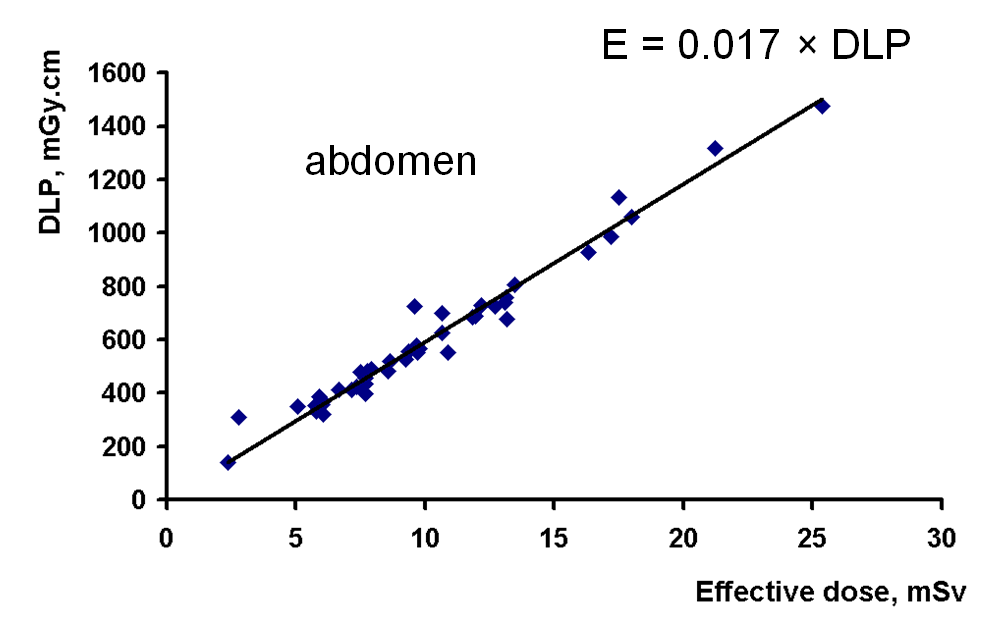
As mentioned above, the DLP is a metric which is related to the total energy imparted in the patient. Therefore, when reading a radiology report which has both the CTDIvol and DLP listed, the DLP value has a more direct bearing on the overall radiation risk of the procedure. Indeed there is a linear relationship between the effective dose and the DLP, as shown in the above plot.
What is Effective Dose?
The effective dose is a quantity which is a risk metric, and is not a dosimetric quantity per se. The computation of effective dose is performed by estimating organ absorbed doses (for a list of 15 different organs), and then multiplying each of those by a tissue weighting factor. The tissue weighting factors were computed from radiation epidemiological data, and takes into consideration that some organs (e.g. breasts, stomach, lung) are more radiosensitive than others (e.g. brain, skin). The total effective dose is the sum of all of these products.
While it is technically possible to compute the effective dose for a specific patient, the effective dose concept was not designed for individual risk assessment.
Other factors to consider
The California law requiring dose reporting in CT has made everyone more aware of radiation dose issues in CT. The Department of Radiology at UC Davis Medical Center uses a number of different dose-optimization technologies to assure that the radiation dose levels used on our several CT scanners are well tuned to each patient’s CT examination.
There are a number of ways to assure that a CT scan provides a maximum benefit/risk ratio to the patient:
(1) When a physician recommends that a patient have a CT scan, make sure that it is necessary and appropriate. The American College of Radiology publishes appropriateness criteria for a large number of imaging procedures. Radiologists are trained to recognize the most appropriate imaging study for a given patient’s circumstances, and consultation with a radiologist can provide guidance in many cases.
(2) In certain circumstances, other imaging modalities such as ultrasound (US) and magnetic resonance imaging (MRI) that do not use ionizing radiation can be used instead of CT. However, not all CT examinations can be replaced with US or MRI.
(3) Younger patients (<30) are more radiosensitive than older patients (>40), and this fact should be considered when a CT scan is recommended.
All medical tests have risks as well as benefits, and CT is no different. When used appropriately, diagnostic CT imaging can provide important diagnostic information which improves patient care and patient outcomes. Before the advent of CT, exploratory surgery was a relatively common procedure, even with its considerable risk and associated pain. CT is a pain-free test which allows doctors to look around the patient’s internal anatomy. The diagnostic information from the CT procedure in many cases provide physicians critical information which can lead to optimal treatment strategies.
References
The Essential Physics of Medical Imaging, 3rd Edition, Lippincott Williams and Wilkins (2012) Bushberg, Seibert, Leidholdt and Boone
AAPM Report 204, Size Specific Dose Estimates (SSDE) in Pediatric and Adult Body CT Examinations, www.aapm.org/pubs/reports/rpt_204.pdf (free to all)
[1] Such as radiation therapy treatment planning, attenuation correction in positron emission tomography scans, and CT imaging used for biopsy needle guidance.
[2] Effective diameter is determined from a circular area that has the same area as the patient cross-section, typically measured at the midpoint of the scan length. This also can be determined from the CT localizer scan as described in reference [3].
[3] Compared to the finger, the abdomen received 1/10 of the dose to 2500 times the tissue mass, resulting in 250 times more absorbed energy than the finger. The total absorbed energy is called the energy imparted.
