Department of Medical Microbiology and Immunology
Departmental Mission
 Our Mission is to develop new approaches for the prevention and treatment of infectious diseases and immunologic disorders. Department programs are integral to the School's new Initiative on Infectious Diseases. Researchers use state-of-the-art technologies of genomics, proteomics and imaging to study the genes and proteins of the pathogens and their hosts to identify novel targets for prevention and therapy.
Our Mission is to develop new approaches for the prevention and treatment of infectious diseases and immunologic disorders. Department programs are integral to the School's new Initiative on Infectious Diseases. Researchers use state-of-the-art technologies of genomics, proteomics and imaging to study the genes and proteins of the pathogens and their hosts to identify novel targets for prevention and therapy.
California Faces Increased Risk of Valley Fever This Summer
KQED's The California Report
 Following the state’s record-breaking rainfall in the winter, and now its dry heat, public health officials are worried about an uptick in Valley fever infections. Reporter: Izzy Bloom, The California Report
Following the state’s record-breaking rainfall in the winter, and now its dry heat, public health officials are worried about an uptick in Valley fever infections. Reporter: Izzy Bloom, The California Report
Stepping up to the challenge and Making a Difference
MMI Stepping up to the challenge and Making a Difference: Dr. Jose Torres is teaching a New Course on Human Virology

MMI Department faculty have stepped up to the educational challenges of building a pipeline of future virologists, infectious disease researchers and public health experts. Dr. Jose Torres has developed a new undergraduate course, “Human Virology” and is teaching it for the first time, this winter quarter (2022).
This course provides insights into the principles of medical virology, current and future viral pandemics and is relevant for undergraduate students who intend to pursue a career in medicine, public health, and biomedical research. Dr. Torres is passionate about mentoring and supporting undergraduate students and their education in medical virology and public health.
What’s Happening in Medical Microbiology and Immunology
Chancellor’s Award for Excellence in Mentoring Undergraduate Research in the Post Doc/Scientist
 April Ferre, Ph.D.
April Ferre, Ph.D.
April Ferre, Ph.D., lab manager for Dr. Barbara Shacklett's lab, has received the prestigious Chancellor’s Award for Excellence in Mentoring Undergraduate Research in the Post Doc/Scientist Category.
April was nominated for this award by our outstanding Undergraduate Researcher in the Global Disease Biology Program, Jacqueline Lu, who was also nominated for a student research award for her work on T-cell activation in COVID-19 infection.
The award includes a $500 prize which will be given to April at the Spring Awards Ceremony and Reception honoring all Chancellor’s Award winners on Tuesday, June 6, 2023.
Congratulations, April!!









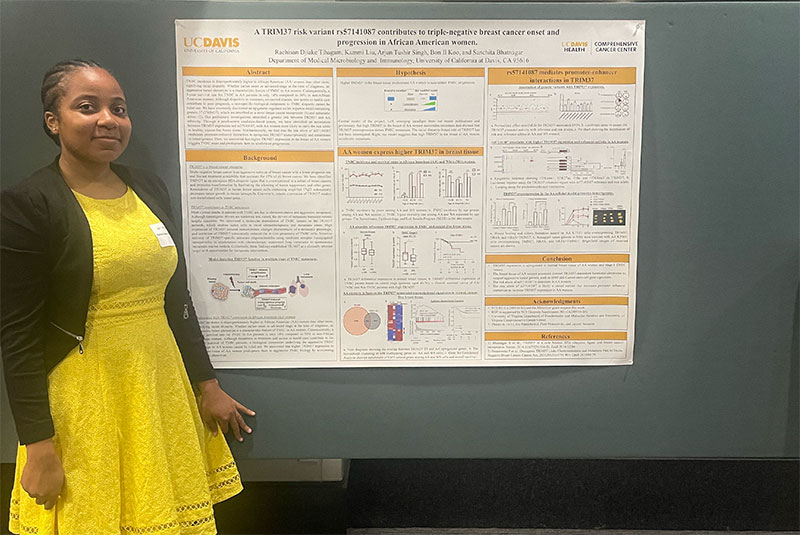 Congratulations Rachisan Dijake (Sanchita Bhatnagar Lab)!
Congratulations Rachisan Dijake (Sanchita Bhatnagar Lab)! Congratulations to Ms. Ramatoulaye (“Rama”) Ouattara
Congratulations to Ms. Ramatoulaye (“Rama”) Ouattara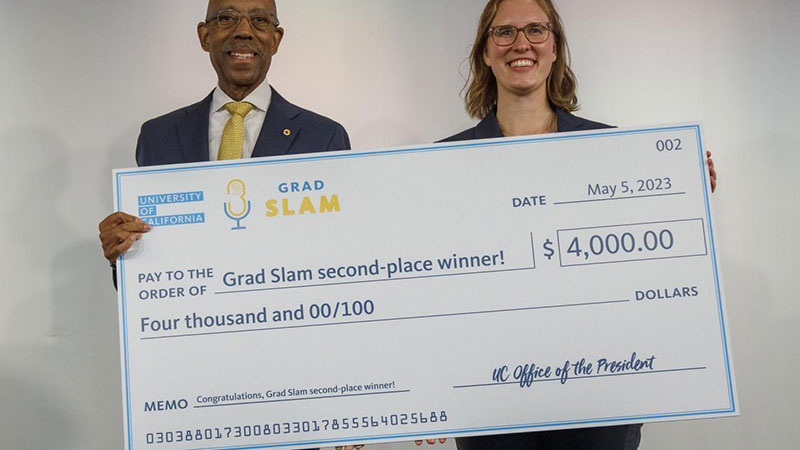 UC Davis Graduate Student, Julia Mouat (Janine LaSalle lab) Wins 2nd Place in UC Grad Slam
UC Davis Graduate Student, Julia Mouat (Janine LaSalle lab) Wins 2nd Place in UC Grad Slam