Study finds disparities in diagnosis and treatment of dementia
Some racial and ethnic groups less likely to receive an accurate and timely diagnosis or anti-dementia medication
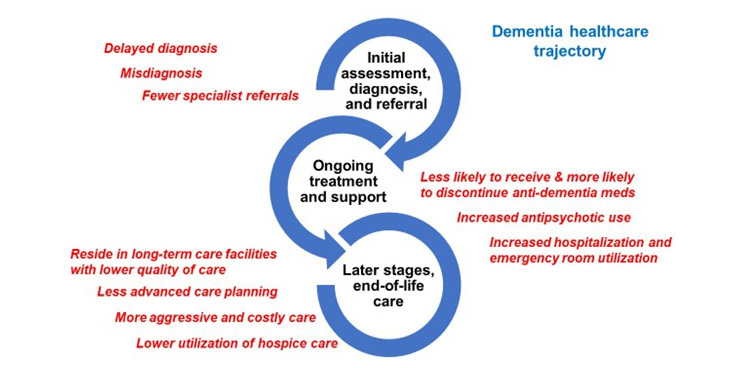
A new study from UC Davis Health and Oregon Health & Science University reveals significant disparities in dementia care. The researchers found that people living with dementia from minoritized racial and ethnic populations are less likely to receive an accurate and timely dementia diagnosis compared to non-Hispanic whites. They were also less likely to be prescribed anti-dementia medication or use hospice care.
In addition, the study found the same populations have a higher risk of hospitalization and receive more aggressive life-sustaining treatment in end-of-life care. The study was published in Alzheimer's & Dementia: The Journal of the Alzheimer's Association.
"Reducing disparities in Alzheimer’s disease and related dementias and receiving timely, high-quality health care services is essential to advance health equity,” said Ladson Hinton, first author of the study and a professor in the UC Davis Department of Psychiatry and Behavioral Sciences. Hinton is also associate director for research in the Family Caregiving Institute at the Betty Irene Moore School of Nursing at UC Davis.
The researchers conducted a scoping review, identifying and analyzing the results of 71 research studies conducted between 2000 and 2022. The studies examined health care access and quality for people with dementia and their caregivers. The studies reported findings related to race and ethnicity.
“Our review provides timely and compelling evidence of disparities in health care quality and access for people living with dementia from minoritized populations,” Hinton said. “It also highlights significant gaps in data, particularly for Asian Americans and Pacific Islanders and American Indians and Alaska Natives populations
Statistically significant differences
Of the 71 studies identified, all but one reported one or more statistically significant differences between racial and ethnic groups. For example:
- 85.9% of the studies reported findings for Black Americans
- 57.7% for Hispanic Americans
- 25.4% for Asian Americans and Pacific Islanders
- 2.8% for American Indians and Alaska Natives
- 32.4% reported aggregate categories for non-white populations
The most frequently addressed topics in the papers were medication treatment (38%), end-of-life care (22.5%), health service use (18.3%), diagnosis (15.5%), family caregiving (7%) and long-term care (5.6%).
Some of the key findings related to diagnosis and treatment found that compared with non-Hispanic white Americans:
- Minoritized populations received less optimal care and experienced delays in how long it took to receive a diagnosis. In one large, recently published study, it took 11% longer for Black Americans and 40% longer for Hispanic Americans.
- Asian American older adults were less likely to receive a diagnostic work-up for cognitive impairment.
- Black and Hispanic American patients were less likely to be referred for neuropsychological testing.
- Minoritized populations had lower rates of prescriptions for anti-dementia medications like cholinesterase inhibitors and memantine.
- Hispanic and Black American older adults had higher discontinuation rates of anti-dementia medications.
Disparities in end-of-life care
There were also disparities in living conditions and end-of-life care. Compared with non-Hispanic white Americans:
- Black Americans with dementia were more likely to have increased hospital admission rates, longer lengths of stay and higher costs.
- Minoritized populations living with dementia were less likely to be in long-term care facilities with special memory care units.
- Caregivers of Black Americans with dementia were less likely to fill out advanced care directives.
- Black Americans with dementia were less likely to receive hospice care and more likely to receive feeding tubes and mechanical ventilation during end-of-life care.
“The results of our study highlight the importance of granular data collection on race and ethnicity,” said Oanh Meyer, co-author and associate professor in the UC Davis Department of Neurology. “Understanding where the disparities exist will help us address why they occur and how to remedy them at the individual, clinical and health-system level.”
Achieving equity and closing gaps in health outcomes
The researchers recommend monitoring for disparities at the local level, educating and training clinicians to reduce bias and improve communication, and enhancing the cultural and linguistic competence of clinical care. They also support developing targeted initiatives to empower people with dementia and family caregivers as they navigate the health care system.
The authors also point out that recognizing existing disparities can prompt policy change at the health system level to address systemic racism and promote health equity.
The researchers noted several limitations of their study, including that some studies may have been missed for inclusion and that the underlying factors responsible for the identified differences are unclear and need further research. They note the study also did not include other potential disparities for people with dementia, such as those identifying as LGBTQ, or geographical inequities faced by those living in rural, urban, and suburban areas.
”Ultimately, it’s critical that the best available dementia care is attainable and offered to all Americans, particularly those who are left out of novel research innovations because of their race, social standing or place of residence,” said Ana R. Quiñones, senior author of the study and an associate professor at Oregon Health & Science University. “To make real progress in achieving equity and closing the gaps in outcomes for Alzheimer’s disease and related dementias, we must do more to ensure the most promising interventions are aimed at those who need them the most.”
Additional authors of the study include Duyen Tran at UC Davis Health and Kate Peak at Oregon Health & Science University.
Funding for this study was supported by the National Institute on Aging (U54AG063546).
Resources
Related stories