Treatment Options for Lymphedema
UC Davis offers a personalized, comprehensive treatment program to help patients who have or are at risk for lymphedema based on each individual’s history, symptoms, test results and goals. Treatment options offered at the UC Davis Center for Lymphatic Disease can be generally divided into surgical treatments (lymphatic surgery) or conservative treatments (therapy):
Lymphatic Surgery
The UC Davis Center for Lymphatic Disease evaluates patients for state-of-the-art surgical interventions such as lymphovenous bypass, lymph node transplantation, and debulking procedures to treat lymphatic disorders.

Lymphovenous Bypass (LVB) surgery uses a high-powered microscope and very fine surgical tools to connect lymphatic vessels that have a blockage to nearby veins which allows for your lymphatic fluid to be redirected past the blockage and flow away from your affected limb.
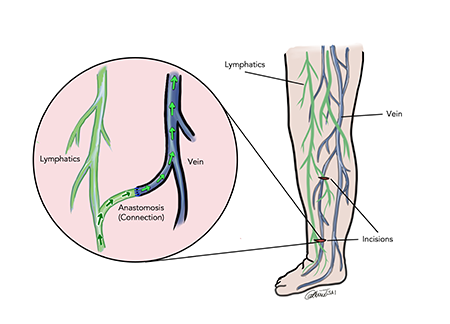
Lymphovenous bypass is typically an outpatient procedure (this means you go home the same day of surgery and do not need to stay in the hospital). The procedure usually requires general anesthesia (you are fully asleep) and involves anywhere between 1-4 very small incisions (2-4cm in length) on your affected extremity. Most patient only need Tylenol for pain control after surgery. This procedure requires careful coordination with your lymphedema therapist for bandaging before and after your surgery.
Lymph node transplantation procedure involves removing healthy lymph nodes and vessels from another area of your body and implanting them into the arm or leg affected by lymphedema using a process called microsurgery. These transplanted lymph nodes help move fluid that has been stuck in the affected arm or leg.
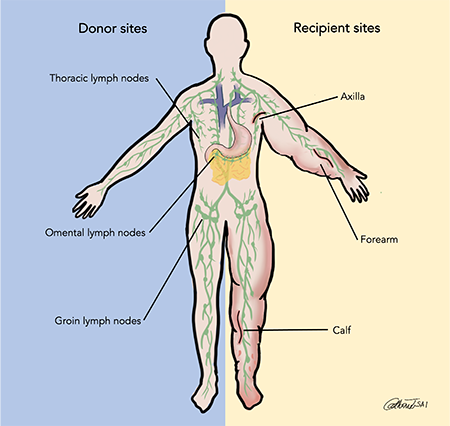
Vascularized lymph node transplant is an inpatient procedure (this means you are admitted to the hospital after surgery). Patients typically stay a few days in the hospital for upper extremity surgery and around a week in the hospital for lower extremity surgery. Incision locations depend on where the lymph nodes are removed from for transplantation – these sites are called “Donor Sites”. Common donor sites include the groin or the chest wall under the arm. Lymph nodes can also be taken from an organ called the omentum inside the abdomen with the assistance of surgeons with special training in laparoscopic surgery (only requires a few small incisions on your abdomen). “Recipient Sites” refer to the areas where these lymph nodes are placed. These sites vary depending on your symptoms. For upper extremity lymphedema, lymph nodes are typically placed in the forearm or under your arm (axilla or armpit). For lower extremity lymphedema, they can be placed in the calf or your thigh, depending on your symptoms.
SAPL is a type of debulking procedure that addresses the buildup of fat that can occur with more advanced lymphedema. During this procedure, excess fat accumulated in the arm or leg affected by lymphedema is removed through liposuction. The reduction in the size of the extremity is maintained long-term with compression. The results from a liposuction debulking procedure are realized immediately.
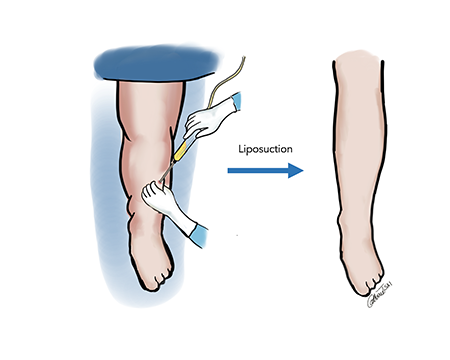
SAPL is typically an outpatient procedure (this means you go home the same day of surgery and do not need to stay in the hospital). The procedure requires general anesthesia (you are fully asleep) and involves multiple small 1cm incisions on your affected extremity. This procedure requires careful coordination with your lymphedema therapist for bandaging before and after your surgery. Depending on the amount of excess fat in a limb or limbs, more than one liposuction procedure may be necessary.
Prehabilitation for Lymphatic Surgery
Completing a full course of complete decongestive therapy prior to surgery is important to assure optimal outcomes post-operatively. Your lymphedema therapist and surgeon will work with you to determine the best plan of care. Engagement in prehabilitation will also prepare you for continued lymphatic therapy after surgery.
Lymphatic Therapy
Our lymphedema therapists have all received advanced certification in manual lymphatic drainage techniques and lymphedema treatment. Specialized lymphedema therapists can teach you about techniques and equipment that can help reduce lymphedema swelling. Examples include:
- Exercises: Gentle contraction of the muscles in the arm or leg can help move the excess fluid out of the swollen limb.
- Manual lymph drainage: Therapists trained in this massage-like technique use very light pressure to move the trapped fluid in the swollen limb toward an area with working lymph vessels. People should avoid manual lymph drainage if they have a skin infection, blood clots or active cancer in the affected limb.
- Compression bandages: Using low-stretch bandages to wrap the entire limb encourages lymph fluid to flow back toward the trunk of the body.
- Compression garments: Close-fitting elastic sleeves or stockings can compress the arm or leg to encourage lymph fluid drainage. These garments often require a prescription to ensure that the proper amount of compression is used. You may need to be measured by a professional to ensure proper fit.
- Sequential pneumatic compression: A sleeve worn over the affected arm or leg connects to a pump that intermittently inflates the sleeve, putting pressure on the limb and moving lymph fluid away from the fingers or toes.
- Meticulous skin care: Good hygiene and proper moisturizing can help prevent injury and infection.
Complete Decongestive Therapy
Complete decongestive therapy (CDT) is the gold standard for lymphedema treatment. CDT consists of two phases – a reduction phase, followed by a maintenance phase. The reduction phase focuses on reducing the amount of swelling a part of the body and softening fibrotic or harden tissue. Once the reduction in the amount of swelling has plateaued, there is a transition to the maintenance phase. The maintenance phase may be for years or life-long, although adjustments may be needed.





