Resident Program - Case of the Month
October 2018 - Presented by Dr. Ying Liu (Mentored by Dr. Anthony Karnezis)
Discussion
This is an example of metastatic signet ring cell carcinoma. In general, primary mucinous carcinomas of the ovary are extremely rare, it comprises 2–3% of ovarian epithelial neoplasms. Signet ring cell mucinous carcinomas of the ovary are mostly metastases of primary tumors from stomach, pancreas, appendix, colorectal or biliary tract. Other rare primary tumor sites have also been reported such as renal pelvis, bladder, uterus or breast tumors with signet ring cell differentiation.
Gross and microscopic features suggest metastatic signet ring cell carcinoma include bilateral involvement, modest ovarian enlargement (commonly < 10-13 cm), nodular superficial growth, and irregularly infiltrative glands with a haphazard distribution, surface tumor implantations, extraovarian extension and lymphovascular invasion. Occasionally, however, metastases can be large, unilateral, which mimic the histological appearance of a primary ovarian tumor. Oftentimes, the primary malignancy is not known at the time of surgery. Primary tumors in the colon, appendix, stomach etc. are often found. In the current case, the ovarian tumors are bilateral and borderline in size (14 cm on the right and 9 cm on the left). Careful intra-operative exploration revealed an appendiceal mass.
Histologically, ovarian tumor show signet ring cells forming small glands, infiltrating as individual cells or small clusters. Immunohistochemistry may be applied as an additional method to help distinguish between primary and metastatic mucinous carcinoma of the ovary. In the current case, negative PAX8, together with the gross and microscopic appearance of the ovaries, is against a primary ovarian mucinous carcinoma (though PAX8 is not expressed in many primary ovarian mucinous carcinomas). The CK20/CDX2 positive, CK7 negative status, together with the gross and microscopic appearance of the appendix, indicate it is the site of origin. The negative synaptophysin and chromogranin are against origin in a goblet cell carcinoid tumor. Intact DNA mismatch repair profile (Intact nuclear expression of MLH1, PMS2, MSH2, MSH6) does not support for lynch syndrome or other hereditary cancer syndrome.
Differential Diagnosis
Primary ovarian mucinous carcinoma: Most arise in a benign or borderline tumor. Primary tumors are usually unilateral, > 10 cm, smooth capsule with cystic and solid areas of tumor evenly distributed throughout ovary without discrete nodularity. Stromal invasion shows solid growth, atypia, stratification, papillae, loss of glandular architecture and necrosis. The two patterns of invasion are expansile and infiltrative. One should also be aware, immunophenotypes of a primary and metastatic ovarian mucinous tumor from the stomach, appendix, or colorectum, may overlap. PAX8, although while widely expressed in non-mucinous primary ovarian carcinoma, expressed in less than 50% of primary ovarian mucinous carcinoma. Thus, negative PAX8 does not rule out mucinous carcinoma. Therefore, thorough gross inspection, clinical history and radiological and histopathological correlations should be considered to ensure correct diagnosis.
Goblet cell carcinoid tumor: Goblet cell carcinoid is a rare tumor almost exclusively involving the appendix. The tumor is thought to arise from pluripotent intestinal epithelial crypt-base stem cells underwent neuroendocrine and mucinous differentiation. Patients usually present in the fifth to sixth decade. They present with acute appendicitis, abdominal pain and a mass. Half of the female patients present with ovarian metastases. The unique histologic feature is clusters of goblet cells in the lamina propria or submucosa, that stain positive for neuroendocrine markers. Recently molecular studies have shown these tumors have some changes similar to that of ileal carcinoids (allelic loss of chromosome 11q, 16q and 18q) but lack the signatures of adenocarcinoma. For the current case, tumor cells stain negative for chromogranin and synaptophysin. Thus, the morphological features and immunohistochemistry stains have excluded appendix goblet cell carcinoid tumor.
References
Kim JH, Cha HJ, Kim K-R, Kim K. Primary ovarian signet ring cell carcinoma: A rare case report. Molecular and Clinical Oncology. 2018;9(2):211-214. doi:10.3892/mco.2018.1653.
Seidman JD, Kurman RJ, Ronnett BM. Primary and metastatic mucinous adenocarcinomas in the ovaries: Incidence in routine practice with a new approach to improve intraoperative diagnosis. Am J Surg Pathol. 2003;27:985–993. doi: 10.1097/00000478-200307000-00014.
McCluggage WG, Young RH. Immunohistochemistry as a diagnostic aid in the evaluation of ovarian tumors. Semin Diagn Pathol. 2005;22:3–32. doi: 10.1053/j.semdp.2005.11.002.
http://www.pathologyoutlines.com/topic/ovarytumormucinouscarcinoma.html
Chai H-J, Ren Q, Fan Q, et al. PAX8 is a potential marker for the diagnosis of primary epithelial ovarian cancer. Oncology Letters. 2017;14(5):5871-5875. doi:10.3892/ol.2017.6949.
Roy P, Chetty R. Goblet cell carcinoid tumors of the appendix: An overview. World Journal of Gastrointestinal Oncology. 2010;2(6):251-258. doi:10.4251/wjgo.v2.i6.251.
Ordonez NG. Value of PAX 8 immunostaining in tumor diagnosis: a review and update. Adv Anat Pathol. 2012;19: 140–151. pmid:22498579

 Meet our Residency Program Director
Meet our Residency Program Director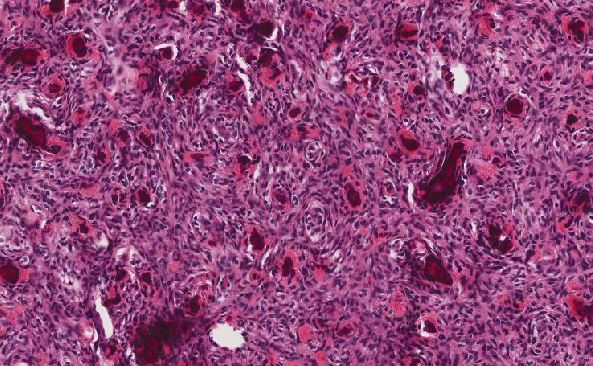
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May