As Americans live longer and their complicated health challenges increase, UC Davis Health has combined geriatric-focused specialties into a new Division of Geriatrics, Hospice and Palliative Medicine. To lead the new effort is Rebecca Boxer, M.D., M.S., a geriatrician and researcher who has dedicated her life to the care of this population.
In a 2022–23 survey of nearly 5,000 medical centers nationwide, U.S. News & World Report ranked UC Davis Medical Center 23rd in the nation for geriatrics based on patient outcomes, key programs and above-average patient experience. UC Davis Health has also achieved age-friendly designations and developed specialized services focused on older adults. Boxer looks to expand that focus and expertise.
“I chose to come to UC Davis Health because of the system-wide commitment to age-friendly health care. A committed system means that programs and health care initiatives for older adults can truly be realized,” Boxer said. “My hope is to provide excellent care to my patients and collaborate across disciplines, to teach all levels of learners the nuts and bolts of caring for older adults. I also want to be a conduit for national opportunities for faculty interested in aging research.”
Boxer is a geriatrician caring for older adults with multiple chronic conditions, functional decline, dementia, and frailty, and has broad research interests including heart failure management, nursing home care, polypharmacy and social determinants of health. She primarily conducts pragmatic clinical trials and often collaborates with investigators in other specialties and disciplines; prior to joining UC Davis Health, she served as medical director of clinical trials at Kaiser Permanente Institute for Health Research in Colorado.
New division streamlines services, attracts new faculty
An estimated 30% of people over 65 need a physician specializing in geriatrics. The new division, housed in the UC Davis School of Medicine’s Department of Internal Medicine, aims to streamline and strengthen geriatrics, hospice and palliative medicine and provide leadership for the rest of the health system. Additionally, the division creates a home that will attract new faculty, new programs and funding in aging medicine.
“We recognize the incredible value of specialized geriatrics professionals who focus on the needs of providing care for older adults,” said internal medicine chair Timothy Albertson, M.D., M.P.H., Ph.D. “They can be the drivers who ensure the rest of the health care team understands the unique needs of these patients and trains the future generation of providers.”
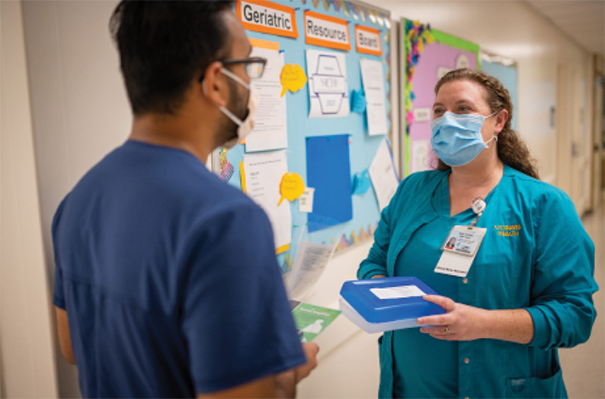
Geriatric, hospice and palliative care experts provide interdisciplinary team-based care for frail, multi-complex older adults across care settings. Merging the three areas is critical to aligning care needs of older adults, and reduces unnecessary hospital or Emergency Department visits.
The new division is also home for scholarly work, and education in clinical work and aging-related research. Boxer looks to grow her team of new geriatricians to join UC Davis Health.
Program addresses geriatrician shortage
According to a federal model, a single geriatrician has the capacity to provide medical care for 700 patients with complex needs. While it’s projected the nation will require 33,200 such physicians by 2025, currently there are only about 7,000 — with only half practicing full-time.
Boxer sees patients in UC Davis Health’s Healthy Aging Clinic, where a multispecialty team offers services such as cognitive neurology, neuropsychology, nursing, dietary planning, pharmacy, and social work for patients 65 and older and their caregivers. Boxer also serves on the executive team of the Healthy Aging Initiative, UC Davis Health’s system-wide commitment to age-friendly services that increase access to care, improve quality of life and make navigating the care system easier. Those efforts have earned Age-Friendly Health System Committed to Care Excellence designations for UC Davis in the inpatient, outpatient and Emergency Department settings.
A 2018 analysis revealed that, from the academic year of 2001-02 to 2017-18, the number of graduate fellowship programs that train geriatricians and are supported by Medicare increased from 182 to 210. However, when accounting for U.S. population growth, this increase is negligible.
Boxer’s team collaborates with clinicians, researchers, and educators at the School of Medicine, the Betty Irene Moore School of Nursing at UC Davis and its Family Caregiving Institute, which focuses on preparing caregivers and health providers to work together, and developing support systems. In addition to several geriatric-focused fellowships, Boxer hopes to further integrate geriatrics content into the School of Medicine curriculum.
The next 40 years
Sacramento’s population is growing older, more quickly. According to census figures, the share of residents aged 65 or older in the region grew by more than half from 2010 to 2020 — the fastest rate in 130 years.
While the latest census data did not surprise Boxer, one statistic does alarm her. According to the California Department of Aging, the region’s population of adults over age 85 is expected to increase 400% by 2060. That underscores the need for a multi-pronged approach to care.
“Our new division serves as an academic home for passionate clinicians and innovative researchers to hopefully allow people to live healthier lives in their communities,” she said. “We must have an environment that helps people stay healthy as they age, while we care for the older frail person needing more services.”





