Residual Nodule, Cavity And Chronic Infiltrates
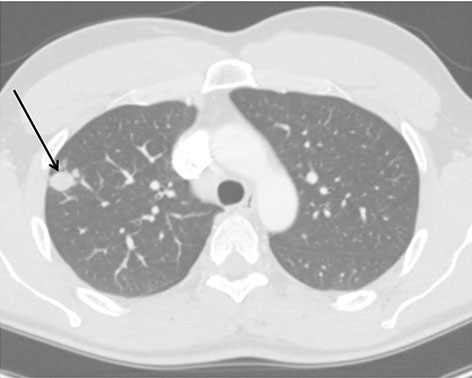
Residual nodule following resolution of primary infection.
Approximately 5% of patient with resolution of primary pneumonic infiltrate can develop a pulmonary nodule or cavity. The initial identification of a coccidioidal infection could be a pulmonary nodule or cavity found incidentally on imaging studies. Nodules due to Coccidioides are often difficult to differentiate from malignancy, especially in persons who have not been diagnosed with coccidioidomycosis previously. Positron emission tomography (PET/CT) has been employed but is not always able to differentiate malignancy from coccidioidal pulmonary nodule(s). In an endemic region of California with a lung nodule program, approximately one-third of nodules are attributable to Coccidioides. Certain factors may have increased association with a coccidioidal nodule rather than malignancy; including male sex, age <55, lack of underlying pulmonary disease, farm labor or construction occupations, a nodule < 2 cm in size, and a nodule described as diffuse or smooth in appearance (1). Immunologic assays may be less reliable in this setting and often a bronchoscopy or biopsy is required to establish the diagnoses via histopathology, culture, and possibly PCR. Asymptomatic nodules attributed to coccidioidomycosis do not require treatment. When such lesions are stable over time with repeated radiographic imaging over 2 years in combination with a benign clinical course, no intervention is necessary. Any treatment decision should take into account patient risk factors, serologic studies, and characteristics of the lesion.
Coccidioidomycois is also known to cause cavitary disease in the lung, ranging from asymptomatic to symptomatic and/or ruptured. While cavities are characteristically described as thin-walled and solitary, the morphology can be variable. Asymptomatic cavities can often be monitored radiographically, and the use of azole therapy is unproven. Symptomatic cavities may cause local discomfort or hemoptysis, and bacterial superinfection is possible. For symptomatic cavities or in those with elevated CF titers, a course of oral antifungals may be considered in order to improve symptoms, but may not result in cavity closure. A more serious complication is a rupture of a cavity into the pleural space causing hydropneumothorax. In such cases, antifungal therapy along with surgical closure by lobectomy with decortication should be considered, especially in younger healthy patients. Initial antifungal therapy can include AmB or azole therapy.
A small percentage of patients may develop chronic fibrocavitary disease which encompasses persistent ongoing symptoms of cough, fever, weight loss, and fatigue lasting for several months. Radiographic findings may show multifocal consolidations with cavitary lesions. Fluconazole or itraconazole are often prescribed for longer durations (a year or longer). If the response is suboptimal despite prolonged therapy, options include increased dosing or changing agents to AmB or an alternative azole. Newer azoles can be tried and have been used successfully (2). Surgical options should be explored in those not responsive to therapy with persistent hemoptysis.
REFERENCES
- Ronaghi R, Rashidian A, Peterson M, et al. Central Valley Lung Nodule Calculator: Development and Prospective Analysis of a Newly Developed Calculator in a Coccidiodomycosis Endemic Area. Presented at 59th Annual Coccidioidomycosis Study Group in San Diego, CA: April 11, 2015.
- Kim MM, Vikram HR, Kusne S, Seville MT, Blair JE. Treatment of refractory coccidioidomycosis with voriconazole or posaconazole. Clin Infect Dis 2011; 53(11): 1060-6.


 Karryn Doyle, CCEP
Karryn Doyle, CCEP