In the past few years, researchers have been gradually illuminating the secret lives of gastrointestinal bacteria, also called microbiota. This is no small task. There are trillions of microbes in the body — ten times more bacteria than there are cells. And while many may perform beneficial tasks, others aren’t so friendly. Researchers believe these bacteria play a role in metabolism, immunity, even mental health. There’s also evidence that certain gut bacteria can influence the risk of developing cancer.
Conditions like type 2 diabetes and obesity can skew this carefully balanced system, increasing levels of hostile bacteria. But it may not even take a disease to throw bacterial ratios out of whack. New evidence suggests that the so-called Western diet — high in sugar and fat — also plays havoc with our microbiota.
Could these bacterial imbalances be contributing to gastrointestinal and liver cancers?
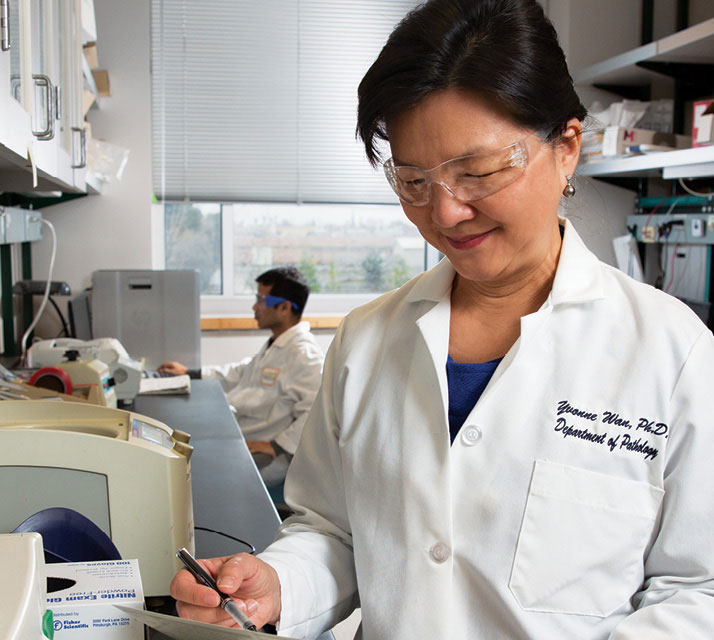
Yu-Jui Yvonne Wan, vice chair for research in the Department of Pathology and Laboratory Medicine, and colleagues are on a mission to find out. They want to determine exactly what role bacteria play in gastrointestinal and liver cancers. But even more importantly, if imbalances in gastrointestinal bacteria raise the risk for cancer, could restoring that balance be the key to preventing it?
The busy liver
That gut bacteria might modulate the risk of liver cancer is not as farfetched as it may seem. While the liver is rightly credited with filtering out many of the toxins people put in their bodies — alcohol being the most notable — that’s only part of the story. The liver and digestive tract are constantly interacting, transporting fluids, nutrients, fat and bile acids, which are crucial to nutrient absorption and other functions.
“The liver carries a heavy load — detoxification, nutrient absorption, fat metabolism,” Wan says. “Plus, it has an extremely close relationship with the gut. Bile acid is made in the liver, circulates to the gut and then comes back to the liver.”
This transaction is of particular interest to Wan and could be the point at which bacteria make their entrance. The liver produces water-soluble, or primary, bile acid, which is transported to the gut. Once there, certain species of bacteria convert this primary bile acid into secondary, water-insoluble, bile acid, which can be toxic.
“In normal amounts, secondary bile acid helps absorb nutrients,” notes Wan. “But everything is about dose. Too much secondary bile acid can damage DNA and activate cancer genes. It also plays a role in inflammation, which can also be carcinogenic.”
A healthy gut regulates the levels of secondary bile acid; however, there is evidence that people with diabetes, obesity and metabolic syndrome tend to have too many of the wrong bacteria. It’s possible these conditions, and the high-fat diets that help generate them, are creating too much toxic bile acid.
The final straw
Livers are complicated and so is liver cancer. Generally, liver cancer patients have had a previous liver condition, such as hepatitis or fatty liver disease, which ultimately leads to cancer. However, some people can have these pre-existing conditions without developing liver cancer.
Researchers have wanted to explain this disparity. What is protecting some people from cancer while others succumb? Once again, the trail leads back to microbiota. It’s possible that unfriendly bacteria, which may generate too much toxic bile acid, are the final elements that push fatty liver disease and other conditions into becoming liver cancer.
“Bile acid may not be directly causing liver cancer, but there’s a lot of evidence that it plays a contributing role,” says Wan.
To figure that out, Wan was recently awarded a $2.7 million grant from the National Cancer Institute. She and fellow grantees Carolyn Slupsky and David Mills, associate professor and professor, respectively, in the UC Davis Food Science and Technology Department and the Foods for Health Institute, will now have the resources to thoroughly investigate the relationship between gut bacteria and both gastrointestinal and liver cancers.
Building on earlier studies, the team hopes to illustrate the relationship between the Western diet, gut bacteria, metabolism and bile acid. With this information, the researchers believe they will produce a better picture of the entire chain of events that lead to liver and gastrointestinal cancers: diet leading to unbalanced gastrointestinal bacteria; increased production of toxic bile acids; inflammation and DNA damage; and cancer gene activation.
Bacteria as medicine
The research will perform another important function: evaluate potential therapies that could disrupt this chain and perhaps even prevent cancer. With all the cross-talk between gut and liver, the possible relationship between unbalanced microbiota and liver cancer provides an intriguing possibility. What if we could rebalance gut bacteria to reduce levels of toxic bile acid?
The idea that we can improve health by introducing friendly bacteria is not new. Probiotics have been touted for their health benefits for many years. More recently, doctors have been using fecal transplants to insert beneficial bacteria into diseased intestines to treat C. difficile, a bacterial infection that’s often hard to treat.
Wan and her team also are interested in using bacteria as medicine. Specifically, they will be testing whether a common gut microbe, called bifidobacteria, along with oligosaccharides (carbohydrates) found in milk, can restore bacterial balance. The bifidobacteria will enrich healthy gut bacteria, while the oligosaccharides will provide food for these good bacteria. The researchers hope this combination will provide a one-two punch, protecting both the liver and gut from inflammation, reducing levels of toxic bile acid, and lowering the risk of gastrointestinal and liver cancers.
“We want to understand the link between bacterial composition and cancer,” says Wan. “But even more importantly, we want to use this approach to intercept the carcinogenic process and, hopefully, reduce cancer formation.”
