Residency Program - Case of the Month
February 2014 - Presented by Christina Di Loreto, M.D.
Answer:
Carcinosarcoma
Microscopic Description:
Histologic sections show a biphasic tumor composed of two distinct malignant cell populations arising within endometrial polyps. There is an epithelial component consisting of back to back endometrial-type glands with atypia, and a separate mesenchymal component made up of sheets of cells with variably shaped hyperchromatic nuclei, numerous mitoses, and occasional giant cells. Immunohistochemical stains demonstrate p16 positivity in the malignant epithelial component and smooth muscle actin (SMA) positivity as well as patchy desmin positivity in the stromal component. With these findings, a diagnosis of carcinosarcoma was made.
Carcinosarcoma:
Carcinosarcoma, formerly known as malignant mixed Müllerian tumor (MMMT), is a biphasic tumor made up of histologically malignant epithelial and mesenchymal elements of Müllerian origin. Once categorized as a uterine sarcoma, it is now recognized as a dedifferentiated metaplastic carcinoma. Carcinosarcomas may arise in the ovary, fallopian tube, cervix, or peritoneum, though this occurs far less frequently than in the uterus.1
Clinical Features:
Two to five percent of all malignancies of the uterine corpus are carcinosarcoma.2-3 This neoplasm typically occurs in postmenopausal women (from sixth to eighth decades, median age 66 years); however, it has been reported in younger women (<40 years of age) and children.2-3 Common symptoms/signs at presentation include abnormal vaginal bleeding, abdominal pain, an abdominal mass, and uterine enlargement.
Carcinosarcoma shares risk factors with endometrioid endometrial adenocarcinoma, including pTEN mutation, obesity, nulliparity, exogenous estrogen, and prior history of pelvic irradiation.2-4 However, the influence of these factors appears to be weaker than in endometrial carcinoma. Tamoxifen therapy may also be included in this list, but the evidence is not conclusive.
Gross Features:
The gross appearance of carcinosarcoma is variable. It may present as a broad-based polyp that fills the uterine cavity or it may cause diffuse enlargement of the uterus, developing into a large mass. The cut surface typically appears smooth and fleshy and may show areas of necrosis, hemorrhage, and cystic change. There may also be hard areas, corresponding to cartilage or bone formation. Myometrial invasion is often present.
Histologic Features:
Histologically, carcinosarcoma shows malignant epithelial and mesenchymal components with distinctive demarcation between the two. The proportion of the tumor that is epithelial versus sarcomatous varies, which underlies the need for extensive sampling of the tumor. The carcinomatous portion may be of any Müllerian type: serous (most common), endometrioid, clear cell, mucinous, or squamous. In the majority of these tumors, the carcinomatous portion is high grade.
The sarcomatous component may be homologous, composed of cell types that are typically found in the uterus (endometrial stromal sarcoma, fibrosarcoma, undifferentiated sarcoma, or leiomyosarcoma), or heterologous, containing cell types not usually found in the uterus, such as malignant skeletal muscle or cartilage (rhabdomyosarcoma, chondrosarcoma, and osteosarcoma).
The immunohistochemical profile of the tumor should correspond to the immunophenotype of the individual elements. The epithelial component may be immunoreactive for vimentin, and the sarcomatous component may express cytokeratins.
Pathogenesis:
The pathogenesis of carcinosarcoma is not well understood, and multiple theories regarding its origin have been proposed:
- The ‘collision’ theory proposes that the epithelial and mesenchymal elements arise independently and collide;
- The ‘combination’ theory suggests that both the epithelial and mesenchymal components result from a common pluripotential cell; and
- The ‘conversion’ theory claims that the sarcomatous element derives from the carcinomatous element by a metaplastic process.1-4
The ‘conversion’ theory is currently the most widely accepted hypothesis. This argument is further supported by studies evaluating p53 and K-ras mutations as well as cytogenetic and immunohistochemical studies of cultured cell lines from carcinosarcomas demonstrating that most carcinosarcomas are monoclonal.1
Treatment and Prognosis:
Stage 1 or 2 carcinocarcinoma is usually treated with total abdominal hysterectomy and bilateral salpingo-oophorectomy with appropriate surgical staging. The role of adjuvant radiation and chemotherapy is not certain, and there is no consensus on what the regimen should be for this disease.
As these tumors are highly aggressive, prognosis is poor. The 5-year survival is reported to be 47% for stage I disease, 36% for stage II disease, 22% for stage III disease, and 10% for stage IV disease.3 Surgical stage and myometrial invasion are the most important prognostic factors, though lack of myometrial invasion does not preclude recurrence. Metastatic and recurrent disease is predominantly carcinomatous, supporting the argument that the carcinomatous component is the driving force and that these tumors are actually metaplastic carcinomas.
References:
- McCluggage WG. Malignant biphasic uterine tumours: carcinosarcomas or metaplastic carcinomas? J Clin Pathol 202;55:321-325.
- Robboy, SJ et al. Robboy’s Pathology of the Female Reproductive Tract. 2nd ed. Churchill Livingston, 2009.
- D’Angelo E, Prat J. Pathology of mixed Müllerian tumours. Best Pract Res Clin Obstet Gynaecol 2011;25:7015-718.
- Arend R, Doneza JA, Wright JD. Uterine carcinosarcoma Curr Opin Oncol 2011:23:531-536.

 Meet our Residency Program Director
Meet our Residency Program Director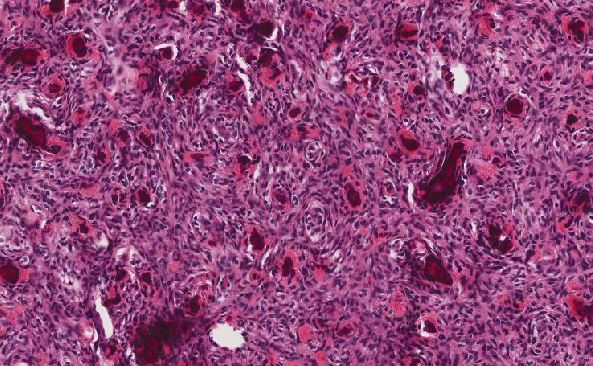
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May