Residency Program - Case of the Month
June 2013 - Presented by Christina DiLoreto, M.D.
Answer:
Whipple Disease
Description of Histology
H&E stained sections show infiltration of the duodenal lamina propria with foamy macrophages and empty round spaces. There is no mononuclear inflammatory infiltrate. Intensely periodic acid-Schiff (PAS)-positive, diastase resistant coarsely granular material is present in the macrophage cytoplasm. Fite stain is negative.
Discussion
Most commonly seen in middle-aged men, Whipple disease is a rare infectious disease caused by the rod-shaped intracellular microorganism, Tropheryma whipplei, a Gram-positive actinobacterium. It can affect multiple organs, including, but not limited to, the gastrointestinal tract, heart, lungs, liver, and central nervous system. Clinical features include weight loss, diarrhea, malabsorption, abdominal pain, fevers, arthralgias, and lymphadenopathy. [1-6] Central nervous system manifestations, such as cognitive dysfunction, oculomasticatory myorhythmia, oculo-facial-skeletal myorhythmia, and cerebellar ataxia may occur. [1] Endocarditis has also been described. [1]
The characteristic histologic findings in the small bowel are expansion of the lamina propria with foamy macrophages that may cause distortion of the villi and adjacent open round spaces (described as dilated lacteals or fat vacuoles). The cytoplasm of the macrophages is filled with diastase resistant, PAS-positive granular material. [2,3,5,6] In the central nervous system, the macrophages surround vessels. [2] Features noted in infected heart valves include significant fibrosis, intermediate-sized vegetations, slight inflammation with foamy macrophages, and lack of calcifications. [1]
The main differential diagnosis is Mycobacterium avium-intracellulare (MAIC) infection, which also shows infiltration by foamy macrophages. Special stains, including AFB stain and PAS with diastase, should be used to distinguish these infectious agents from one another. AFB stain will highlight Mycobacterium, and the PAS stain in MAIC infection will show faintly positive bacillary forms (not globular/granular inclusions like Whipple disease). In addition, the open spaces should be absent in MAIC infection. [3] Other diagnostic considerations include Histoplasma and Rhodococcus. [3] For definitive diagnosis, electron microscopy demonstrating bacillary bodies, polymerase chain reaction (PCR) analysis of T. whipplei 16S ribosomal DNA, or immostaining is needed. [1,2,3,5,6] Culture of this organism is difficult and is not routinely available.
The pathogenesis of Whipple disease has not yet been elucidated. The organism has been identified in healthy asymptomatic individuals, suggesting that host factors play a role in development of the disease. [1,2,4] Gorvel et al suggest that T. whipplei modulates macrophage activation and apoptosis. [4]. Their claims include that macrophages from patients with Whipple disease demonstrate M2 polarization, that T. whipplei replicates in macrophages through an IL-16 dependent mechanism, and that T. whipplei induces macrophage apoptosis through the extrinsic pathway, all contributing to bacterial replication. [4]
Diagnosis of Whipple disease is often delayed due to the rarity of the disease and lack of clinical suspicion. Without treatment, the disease is fatal. Most patients respond well to antibiotic therapy; however, histologic findings may persist, though diminished, and relapse is common, occurring in up to 30% of cases. [2]
References
1. Apstein MD, Schneider TS. Whipple’s disease. Last updated January 10, 2013. <http://www.uptodate.com>
2. Arnold CA, Moreira RK, Lam-Himlin, De Ptris G, Montogomery E. Whipple disease a century after the initial description. Am J Surg Pathol 2012;36:1066-1073.
3. Carter D, Greenson JK, Reuter VE, Stoler MH, Mills SE (Eds). Sternberg’s Diagnostic Surgical Pathology. Fifth Edition. Lippincott William & Wilkins, Philadelphia: 2010.
4. Gorvel L, Al Moussawi K, Ghigo E, Capo C, Mege J-L, Desnues B. Tropheryma whipplei, the Whipple’s disease bacillus, induces macrophage apoptosis through the extrinsic pathway. Cell Death and Disease 2010:e34.
5. Odze RD, Goldblum JR. Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas. Fifth edition. Second Edition. Saunders Elsevier, Philadelphia: 2009.
6. Yajima N, Wada r, Kimura S, Matsuzaki Y, Chiba D, Ebina Y, Ohkusu K, Yagihashi S. Whipple disease diagnosed with PCR using formalin-fixed paraffin-embedded specimens of the intestinal mucosa. Intern Med 2013;52:219-222.

 Meet our Residency Program Director
Meet our Residency Program Director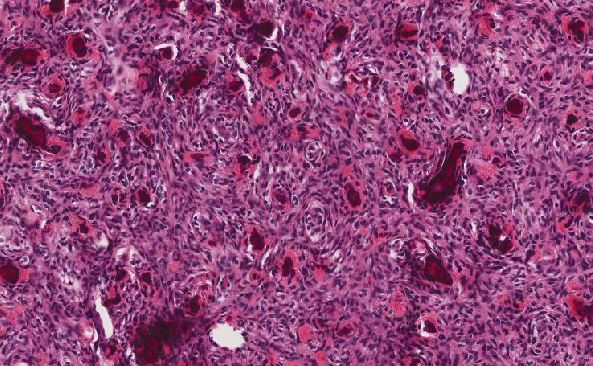
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May