Residency Program - Case of the Month
April 2013 - Presented by Sarah Barnhard, M.D.
Answer:
Cause of Death: Incomplete intestinal rotation with internal herniation
Autopsy findings:
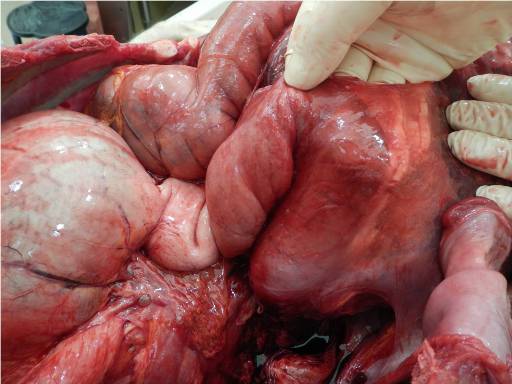
There is massive ischemia of nearly the entire small bowel extending from the distal duodenum to 3cm proximal to the ileocecal valve. There is perforation of the distal ileum and associated 1.4L sanguineous ascites with intermixed food contents. However, there is no evidence of acute peritonitis. The large bowel appears viable. There is an incomplete rotation of the duodenojejunal loop with associated clockwise midgut volvulus. There is distal duodenal (approximate level D3) encasement by a right mesocolic internal herniation and associated Ladd bands which have additionally sequestered 142cm of small bowel. The duodenum does not cross the midline. The cecocolic loop is fully rotated and descended. Appropriate ascending colon and cecal retroperitoneal fixation is indeterminate. The mesenteric base is markedly narrowed and displays prominent ischemic damage.
Autopsy images:
 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
Image 1 - Anterior view of the abdominal cavity, prior to prosection
Image 2 - Right lateral view of small bowel, internally herniated
Images 3 and 4, caption "Encasement of distal duodenum, approximate level D3"
Image 5, caption "Ladd bands extending from ascending colon (lower left). Perforation of distal ileum (forceps)."
Image 6, caption "Ischemic small bowel, reduced from herniated site"
Image 7, caption "Narrowed mesenteric base, in vivo"
Image 8, caption "Near complete ischemic small bowel (proximal duodenum upper left). Viable large bowel (lower left)."
Image 9, caption "Markedly narrowed mesenteric pedicle, ex vivo"
Discussion:
The diagnosis of intestinal malrotation encompasses both nonrotation and incomplete rotation around the superior mesenteric artery (SMA) as well as anomalies of intestinal fixation. Interruption of intestinal rotation and fixation during fetal development can occur at multiple points, leading to a spectrum of both disease severity and acute vs. chronic presentation of the disease.
Malrotation was first reported prior to the 1900s. During the 20th century, embryologic and anatomic science expanded, providing a better understanding of the underlying pathophysiology. In 1936, Dr. William E. Ladd wrote the classic article on the surgical intervention of malrotation (Ladd procedure) and greatly aided the standardization of therapeutic options.
Intestinal malrotation occurs at a rate of approximately 1:500 live births. In addition to being an isolated event, it is also associated with various clinical scenarios including small bowel atresia, Hirschprung disease, GERD, intussusception, persistent cloaca, anorectal malformations, and extrahepatic anomalies. Male predominance is observed in neonates (ratio of ~2:1), but there is no gender predilection in patients over 1 year of age. In some case series, it is estimated that up to 80% of cases present within the first year of life. However, a 17 year retrospective review (1992-2009) at MGH revealed that of 170 cases, 31% were <1 year, 21% were 1-18 years, and the remaining 48% were adults14. Infants more often presented with emesis, whereas adults presented with abdominal pain. The incidence of associated volvulus declined with age, and 32% of adults experienced symptoms for years before diagnosis.
To understand the pathophysiology, it is helpful to have a complete portrait of the normal embryological development of the bowel. Normal rotation occurs around the SMA axis (Figure 16), and involves the proximal duodenojejunal loop (red arrow) and the distal cecocolic loop (green arrow) as the alimentary canal points of rotation. Both loops originate in a vertical plane parallel to the SMA and end in a horizontal plane. Both loops make a total of 270 degrees of rotation around the SMA during normal development.
Normal Intestinal Rotation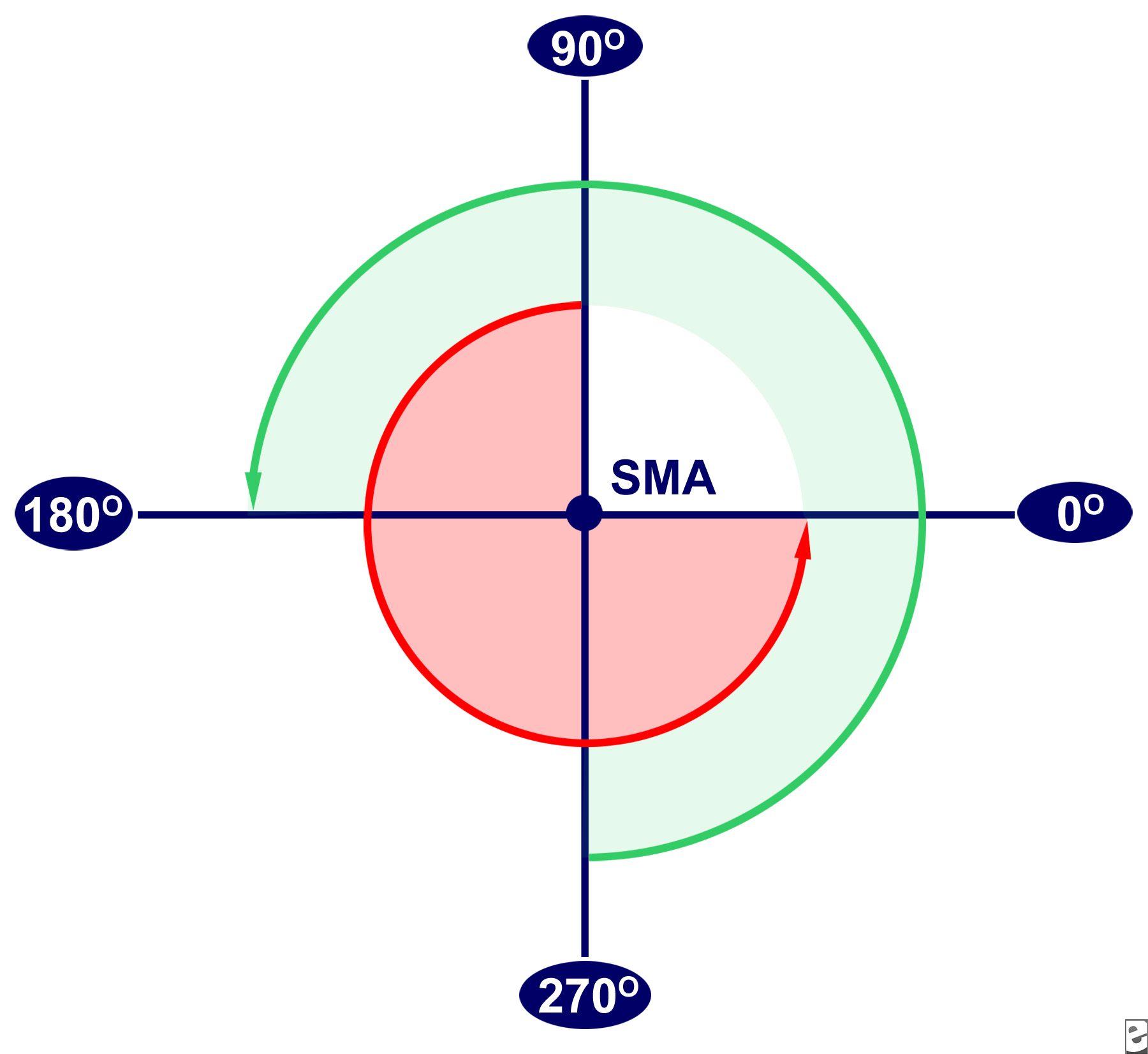
Alimentary development occurs in embryologic stages. Stage I occurs at 5-10 weeks gestational age (GA), and is the period of normal herniation into the base of the umbilical cord. The duodenojejunal loop begins superior to the SMA (at designated 90 degrees on Figure 1) and rotates counterclockwise to the 270 degree position. It ends in a position anatomically inferior to the SMA. The cecocolic loop begins inferior to the SMA and rotates to the 0 degree position, anatomically left of the SMA. These positions are maintained while the midgut lengthens along the SMA and a broad mesenteric pedicle/base is formed. A broad base helps to prevent volvulus.
Stage II occurs at 10 weeks GA, and is the likely stage of duodenojejunal rotation arrest in the decedent. The bowel returns to the abdominal cavity while the duodenojejunal loop rotates an additional 90 degrees to a position anatomically left of the SMA (0 degree position). The cecocolic loop rotates an additional 180 degrees to a position anatomically right of the SMA (180 degree position).
Stage III occurs from 11 weeks GA to full term, and involves the descent of the cecum to the right lower quadrant and fixation of the mesentery.
Overall, the autopsy findings are most consistent with an incomplete rotation due to stage II arrest. In this setting, peritoneal bands extend from the misplaced cecum to the mesentery and compress the third portion of the duodenum. Depending on the level of rotation completed prior to arrest, the mesenteric base may be markedly narrowed, and may incite midgut volvulus as in the decedent. Midgut volvulus is a complication in which clockwise twisting of the bowel around the SMA axis occurs because of the narrowed mesenteric base. It is a clear indication for emergent surgery, but the diagnosis especially in the adult patient is difficult because the presentation is non-specific. Internal herniation may occur if the duodenojejunal loop does not rotate, but the cecocolic loop does. This traps most of the small bowel into the mesentery of the large bowel creating a right mesocolic hernia.
Of interest, an arrest in development at stage I results in nonrotation. In this presentation, the duodenojejunal junction does not lie inferior and to the left of the SMA and the cecum does not lie in the right lower quadrant. The mesentery forms a narrow base as the gut lengthens without rotation. In addition, potential hernia pouches form when the mesentery of the right/left colon or duodenum do not fixate retroperitoneally.
Also of interest is the variable clinical picture of the disease. Internal herniation and chronic midgut volvulus usually have a chronic picture with episodic abdominal pain progressing to constant pain. Vomiting, alternating constipation/diarrhea, abdominal distention, malabsorption syndrome, and GERD may be mistaken for psychosocial issues. Adult patients who present with acute symptoms related to unsuspected malrotation should be rapidly imaged as surgery may be life-saving. However, they may also progress to an acute volvulus too rapidly and present, as in the case of the decedent, with fatality.
References:
- Draus JM Jr, Foley DS, Bond SJ. Laparoscopic Ladd procedure: a minimally invasive approach to malrotation without midgut volvulus. Am Surg. Jul 2007;73(7):693-6.
- Ladd WE. Surgical Diseases of the Alimentary Tract in Infants. N Engl J Med. 1936;215:705-8.
- El-Gohary Y, Alagtal M, Gillick J. Long-term complications following operative intervention for intestinal malrotation: a 10-year review. Pediatr Surg Int. Sep 16 2009.
- Hatley, R et. al. Intestinal Malrotation. Medscape online at http://emedicine.medscape.com/article/930313. Accessed 3/25/13.
- Kamal IM. Defusing the intra-abdominal ticking bomb: intestinal malrotation in children. CMAJ. May 2 2000;162(9):1315-7.
- Kouwenberg M, Severijnen RS, Kapusta L. Congenital cardiovascular defects in children with intestinal malrotation. Pediatr Surg Int. Mar 2008;24(3):257-63.
- Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery. Mar 2011;149(3):386-93.
- Palanivelu C, Rangarajan M, Shetty AR, Jani K. Intestinal malrotation with midgut volvulus presenting as acute abdomen in children: value of diagnostic and therapeutic laparoscopy. J Laparoendosc Adv Surg Tech A. Aug 2007;17(4):490-2.
- Spigland N, Brandt ML, Yazbeck S. Malrotation presenting beyond the neonatal period. J Pediatr Surg. Nov 1990;25(11):1139-42.
- Wanjari AK, Deshmukh AJ, Tayde PS, Lonkar Y. Midgut malrotation with chronic abdominal pain. N Am J Med Sci. Apr 2012;4(4):196-8.

 Meet our Residency Program Director
Meet our Residency Program Director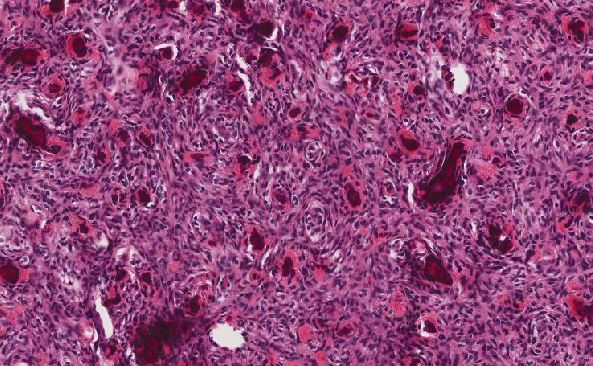
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May