Residency Program - Case of the Month
November 2012 - Presented by Kali Tu, M.D.
Answer:
Clear Cell Adenocarcinoma
Histology:
The sections show a nodular proliferation with a fibrous border. On higher magnification, the nodule is composed of uniform clear cells in a glandular architecture. The cells have clear to foamy eosinophilic cytoplasm and uniform round nuclei with vesicular chromatin and small round nucleoli. Mitotic figure are not identified. There are thin intersection vascular channels throughout the tumor.
Special Stains:
An extensive work up of special stains and immunohistochemical stains were performed to further classify the lesion.
| Pictured | Not pictured | ||
| CK5/6 | Negative | CD56 | Negative |
| CK7 | Positive | CD117 | Negative |
| HMB-45 | Negative | CK20 | Negative |
| Napsin A | Negative | PAX-8 | Negative |
| PAS/PAS-D | Positive | S100 | Negative |
| P63 | Negative | SMA | Negative |
| RCC | Negative | Synaptophysin | Negative |
| TTF-1 | Negative | Vimentin | Negative |
| Mucin | Negative | ||
Discussion:
Clear cell adenocarcinoma of endobronchial origin is rare with only two case reports identified in a Pubmed search [1, 2]. Both of these reported cases occurred in adults, 45 years and 65 years of age. Our case is of a younger adult male of 27 years of age.
The main differential diagnosis in this case is to rule out an adenocarcinoma with focal clear cell features, fetal adenocarcinoma, metastatic renal cell carcinoma, in additional to clear cell (“sugar”) tumor. The immunohistochemical stains being negative for CK5/6 and P63, as well as TTF1 and napsin A would make a diagnosis of either a squamous cell carcinoma or adenocarcinoma with clear cell features unlikely. The renal cell markers are negative. Sugar tumors are classically HMB-45 positive, and therefore our tumor is not in that category. The positivity of CK7 and PAS/PAS-D support an epithelial origin with glycogen positive cytoplasm.
In our case, as well as the two case reports, this type of clear cell adenocarcinoma is known for an endobronchial growth pattern without direct invasion into the underlying parenchyma. Often times the overlying normal bronchial epithelium is normal appearing. This tumor can also spread in a superficial or polypoid pattern. On resection, our tumor showed the same clear cell morphology with similar immunohistochemical staining patters. There were no lymph node metastasis. This is in contrast to the case report by Segawa et al in which there were two lymph nodes positive for metastasis.
The prognosis of clear cell adenocarcinoma is unknown due to its rarity. To date, the patient has been diagnosed, and underwent right lung pneumonectomy. He is less than one-month post-operative and is recovering well.
References:
-
Iyoda, Hiroshima, Toyozaki, Tsukamoto,Haga, Fugisawa, Ohwada. Clear cell adenocarcinoma with endobronchial polypoid growth. Pathol Intern 2000;50:979-83.
-
Segawa M, Seki K, Kusejima Y, Saito K. [Primary clear cell adenocarcinoma of the lung with endobronchial polypoid growth: report of a case]. Kyobu Geka. 2009 Dec;62(13):1182-5.

 Meet our Residency Program Director
Meet our Residency Program Director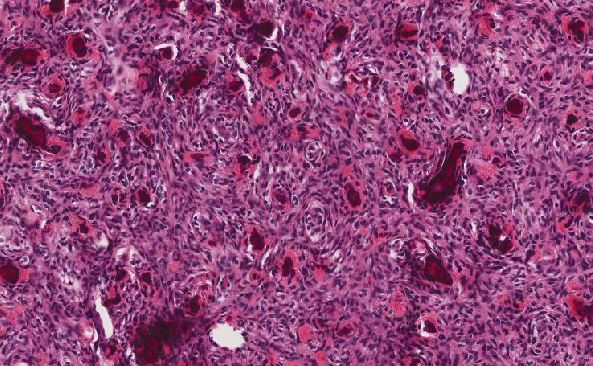
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May