Examples of Marc Dall'Era's Research
Published in Prostate Cancer and Prostatic Diseases:
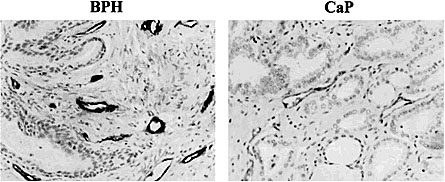
Representative microvessel density in BPH and CaP originating from the same radical prostatectomy specimens (n¼13). Immunohistochemistry with DAB chromogen and hematoxylin counterstain. Our studies show that u-PA is secreted equally by tumor and hyperplastic epithelial components, and to a lesser extent by the stromal cells.
Dall'Era MA, Cowan JE, Simko J, Shinohara K, Davies B, Konety BR, Meng MV,
Perez N, Greene K, Carroll PR.
BJU Int. 2011 Apr;107(8)1232-7.
Abstract
Study Type - Therapy (case control) Level of Evidence 3b OBJECTIVES To compare the pathological outcomes of men undergoing radical prostatectomy (RP) after a period of active surveillance (AS) with those of a similar risk group undergoing immediate surgery. PATIENTS AND METHODS We identified men through our institutional database who underwent RP within 6 months of diagnosis or after a period of AS. The primary outcome of the present study was Gleason upgrade to >/=7 after prostatectomy. Pathological stage and positive surgical margin rate were assessed as secondary outcomes. Binomial logistic regression models were used to determine associations of treatment subgroups with pathological upgrade, upstage and positive margins. RESULTS Thirty-three men with initially low-risk cancer features underwent RP after a median (range) of 18 (7-76) months of AS. A total of 278 men with low-risk disease features underwent immediate RP within 6 months of diagnosis. Rates of Gleason upgrading to >/=7, pathological category pT3 and positive surgical margins did not differ significantly from the immediate RP group. On multivariate analysis of low-risk patients, adjusting for baseline pathological features, treatment group (AS followed by prostatectomy vs immediate prostatectomy) was not associated with Gleason upgrading (odds ratio, OR, 0.35; 95% CI, 0.12-1.04), non-organ-confined disease (OR, 1.67; 95% CI, 0.32-8.65) or positive surgical margins at prostatectomy (OR, 0.95; 95% CI, 0.16-5.76). CONCLUSIONS The present analysis did not show an association between RP after a period of AS and adverse pathological features for men with low-risk disease.
Dall'Era MA, Carroll PR.
Curr Opin Urol. 2009 May;19(3):258-62.
Abstract
PURPOSE OF REVIEW: Prostate cancer is now the most commonly diagnosed solid tumor in American men. Autopsy studies show the uniquely high prevalence rates of small, indolent tumors in men dying of other causes. These findings have led to an increased interest in managing men with prostate cancer and low risk features expectantly, with close observation for early signs of progression. This approach allows one to limit prostate cancer treatment and any risk of related morbidity to the men who will benefit the most from active intervention.
RECENT FINDINGS: Several centers have published their results with active surveillance and delayed selective therapy for men with low grade, early prostate cancer. Although median follow up from these studies is relatively short, the outcomes appear favorable. About one third of men will receive treatment after 3-5 years of surveillance and quality of life remains high.
SUMMARY: Data from these reports provide patients and clinicians with the early experiences and expectations with active surveillance for prostate cancer. They also provide a framework for selecting men for this approach and for following them over time. Prospective, randomized trials comparing active surveillance with standard interventions are underway.
Dall'era MA, Hosang N, Konety B, Cowan JE, Carroll PR.
J Urol. 2009 Apr;181(4):1622-7; discussion 1627.
Abstract
PURPOSE: We determined various sociodemographic predictors of prostate cancer risk category at presentation as assessed by serum prostate specific antigen, cancer grade and tumor stage.
MATERIALS AND METHODS: We performed a retrospective cohort study of 5,939 patients enrolled in the CaPSURE national disease registry database between 1995 and 2007. Prostate cancer risk category was assigned as low, intermediate or high based on diagnostic prostate specific antigen, clinical grade and biopsy Gleason grade. Additionally, a group of men with low grade, limited volume tumors were identified as having clinically insignificant disease. The primary outcome was prostate cancer risk category at presentation. Treatment received vs active surveillance was analyzed as a secondary end point.
RESULTS: Patients who were older, had lower levels of education and had Medicare with or without a supplement instead of private or Veteran's Affairs insurance were more likely to have intermediate and high risk disease than low risk disease. Nonwhite race was associated with high risk disease at presentation. Clinically insignificant disease was more common in men younger than 60 years, those with higher education and income, and those with private insurance. Logistic regression analysis suggested that younger age, higher education and income, and private insurance were related to insignificant disease being detected. Among men with insignificant disease younger age and private insurance were associated with immediate treatment with curative intent.
CONCLUSIONS: Unique sociodemographic variables are associated with the clinical risk of prostate cancer at diagnosis and they may influence treatment decisions and outcomes. Patients with insignificant disease may be susceptible to overtreatment due to the indolent nature of the disease. Intermediate and high risk groups, which are associated with poorer outcomes, may be further endangered by late detection of the disease.
