Bits & pieces
Moonshot grant advances immune therapy for dogs — and one day people — with cancer
UC Davis has received its first National Cancer Institute (NCI) Moonshot grant — $2.5 million over five years — to explore immunotherapy treatments for dogs who develop melanoma and osteosarcoma and that may one day benefit humans, as well.

“These are two cancers that dogs get which are similar to human cancers, and we need new therapies for both of them,” said Robert Canter, a surgical oncologist at the UC Davis Comprehensive Cancer Center and the study’s co-principal investigator. “Both of these diseases often go right to the lungs and have extremely high mortality rates.”
Canter and co-principal investigator Robert Rebhun, a veterinary oncologist and researcher at the UC Davis School of Veterinary Medicine, will combine natural killer cells with cytokines to boost the immune system against cancer cells in 70 dogs with naturally occurring melanoma or osteosarcoma.
“Through Moonshot, the NCI is betting that canine studies will directly translate, inform and improve immunotherapy for human cancer patients,” he said. “This is a ‘win-win’ in that we can investigate promising immunotherapies for pet dogs with cancer that otherwise may be out of treatment options.”
In addition to Canter and Rebhun, investigators include Arta Monjazeb, Michael Kent, William Murphy, Ellen Sparger, Titus Brown, Susan Stewart and William Culp.
Neuropathy after chemotherapy an understudied problem
In two papers published in the Journal of the National Cancer Institute, researchers from UC Davis, UCLA and other institutions found that peripheral neuropathy, which causes pain, numbness, and tingling in hands and/or feet, can bother early-stage breast cancer patients years after completing chemotherapy. In addition, a systematic literature review found only a handful of studies that tracked long-term peripheral neuropathy, leaving little data for patients and clinicians to make informed decisions.
“Until recently, the really strong focus has been to identify treatments to reduce breast cancer recurrence and mortality,” said Joy Melnikow, a co-author who directs the Center for Healthcare Policy and Research at UC Davis. “I think we’ve reached the point now where we need to ask questions about the adverse effects that come along after curative treatments. We need to balance what are sometimes small therapeutic benefits with the risk of long-term adverse events.”
After a systematic review of the literature, researchers found only five papers on studies that followed patients for a year or more. In addition, the research produced widely variable results.
“The most striking finding from the review was how little data was out there,” Melnikow said. “And these studies report a wide range of frequency for peripheral neuropathy, from as low as 11 percent to more than 80 percent of patients at one to three years after treatment.”
The second study was launched to help remedy this scarcity of information. The team looked at 1,512 early-stage breast cancer patients from a large clinical trial that investigated the effectiveness of various combinations of chemotherapies. Overall, two years after the start of treatment, 42 percent of patients experienced neuropathy symptoms and 10 percent reported severe discomfort. In addition, women experiencing more severe neuropathy symptoms reported much worse quality of life.
Oncologists have encouraged patients to receive adjuvant chemotherapy to guard against breast cancer recurrence. However, given the potential for side effects, and the effectiveness of other treatments, the authors concluded that the choice of adjuvant chemotherapy drugs or their avoidance should include consideration of long-term effects of breast-cancer treatment.
“Smart” immune cell research gets boost with Innovator Award
UC Davis Assistant Professor Sean Collins received a $1.5 million award from the National Institutes of Health to advance the development of “smart” immune cells for therapies to treat cancer and other diseases. The five-year NIH Director’s New Innovator Award aims to provide new insight into how to engineer immune cells to control their recruitment and response to tumors.
“Immune cells are emerging as major tools for the next generation of cancer therapies,” said Collins, of the Department of Microbiology and Molecular Genetics and the UC Davis Comprehensive Cancer Center. “Our project is aimed at understanding how immune cells channel information downstream of inputs from the cell surface to control different behaviors.”
One challenge in developing immune cell therapies is to strike a balance between the beneficial anti-tumor responses and negative side effects caused by an amplification of the immune response, such as fever, difficulty breathing, seizures and other problems.
By targeting smart cells to respond in a specific and controlled manner and limiting their ability to amplify the attack signal, Collins hopes the cells will be able to work more effectively to fight tumors and avoid damaging the body’s healthy cells. Taking a systematic, genome-wide approach, Collins’ team will break down the complexity of an immune cell’s signaling network, developing maps that reveal the different response pathways within the cell.
Collins’ award is one of 55 “High Risk, High Reward” New Innovator Awards announced by the NIH in October.
Gandara named ‘Giant of Cancer Care’

David R. Gandara, professor and director of thoracic oncology at UC Davis Comprehensive Cancer Center, was named a “Giant of Cancer Care” in lung cancer by OncLive in recognition of his work to advance the field of oncology through his contributions in research and clinical practice. Gandara was one of 12 inductees at the Chicago History Museum on the first day of the 2017 meeting of the American Society of Clinical Oncology (ASCO) in June, which brings together more than 30,000 oncology professionals from around the world.
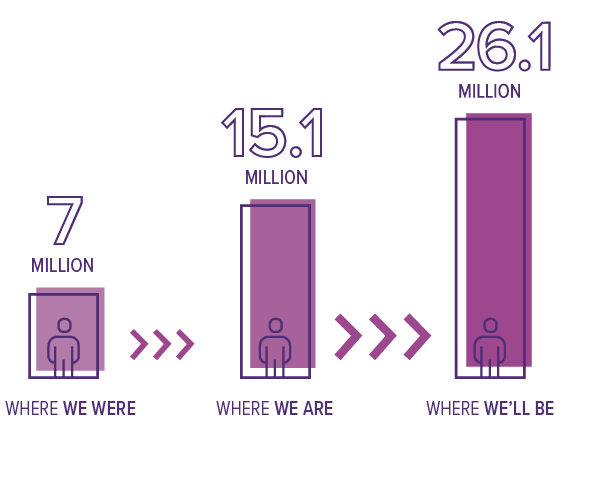
Cancer survivors
Cancer survivorship is on the rise;
by 2040 the number will reach more than 26 million.
A Surge in Older Survivors:
Estimated Number of U.S. Cancer Survivors by Age Group
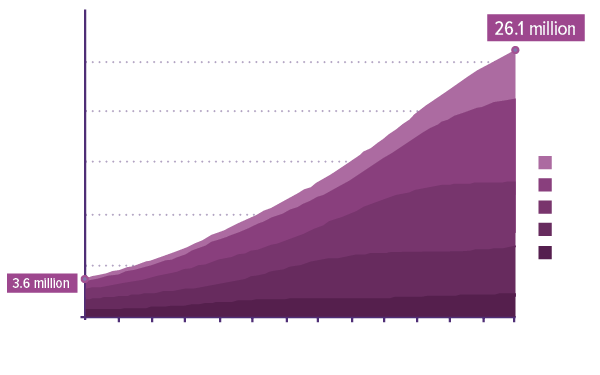
Source: Bluethmann SM et al. Cancer Epidemiol Biomarkers Prev. 2016 Jul;25(7):1029-36. Courtesy of NCI

