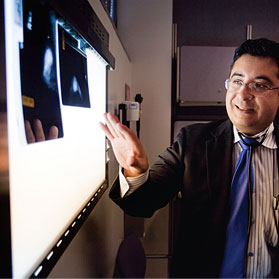
Patient Focus: Cancer surgeon tracks disparities in post-mastectomy breast reconstruction
 As soon as she was diagnosed in January 2009, Shadowens, 42, was determined to get the treatment she both needed and wanted. She found herself in the care of Dr. Steve Martinez, a surgical oncologist at UC Davis Cancer Center. After her second lumpectomy and on Martinez' recommendation, Shadowens opted for a double mastectomy, followed by plastic surgery to reconstruct her breasts.
As soon as she was diagnosed in January 2009, Shadowens, 42, was determined to get the treatment she both needed and wanted. She found herself in the care of Dr. Steve Martinez, a surgical oncologist at UC Davis Cancer Center. After her second lumpectomy and on Martinez' recommendation, Shadowens opted for a double mastectomy, followed by plastic surgery to reconstruct her breasts.
"For me, it was never an option to do nothing. I felt I would feel more normal," Shadowens says. "I didn't even give him a chance to offer reconstruction. I said, 'fix me, and make me look like a woman, not a maimed woman.'"
Recently, she participated in the annual Susan B. Komen Race for the Cure. At least seven women on her race team have battled the disease and have had breast reconstruction after undergoing mastectomy.
This may be because Shadowens and her teammates live relatively close to urban Sacramento. According to a new study by Martinez, breast cancer survivors in more rural counties are less likely than their more urban counterparts to receive breast reconstruction after their mastectomies.
According to a new study by Martinez, breast cancer survivors in more rural counties are less likely than their more urban counterparts to receive breast reconstruction after their mastectomies.
Martinez studied a database with information about the treatment of more than 7,000 Northern California breast cancer patients. Of these, 3,552 had complete information regarding the use of breast reconstruction. All resided in Sacramento and 13 neighboring counties. When Martinez examined where these patients lived, he found stark differences in the extent of treatment they received. Patients from primarily rural counties or counties with only smaller cities, such as Amador, Butte, Stanislaus and San Joaquin counties, were 27 percent to 49 percent less likely to receive breast reconstruction than their urban neighbors.
"Maybe the people who wish not to receive breast reconstruction happen to be the same ones who live in rural areas," says Martinez. "But I have no reason to believe most of those women would live in Alpine or Amador counties; they don't sequester themselves there."
Nor can the difference be ascribed to patient affluence. Insurance companies are legally mandated to cover breast recon-struction after mastectomy, whether or not the care is delivered by a network provider.
Martinez suspects that the disparity boils down to access to care. In outlying areas, medical facilities are probably less likely to offer reconstruction to patients. This might be due to a paucity of plastic surgeons or even a failure to educate patients that the procedure is an option. If the procedure isn't available in local hospitals, women are forced to travel long distances to receive treatment, at a cost of additional time and expense that many cannot afford.
"People say that all politics is local. The same is true for medical care. How you get treated depends on where you are," Martinez says.
Martinez began the study last year after being awarded funds for his breast cancer research by the Amador County Cancer Research Foundation. With a desire to give something back to the community that sponsored him, he decided to examine how Amador County and surrounding areas performed in terms of breast reconstruction. "I wanted to look at the disparities in outlying areas relative to Sacramento," Martinez says. Warren Tseng, a UC Davis general surgery resident, assisted him in the research project.
Martinez called the project the "Sacramento Area Breast Epidemiology Study," or SABES, which is also Spanish for "you know." He considers the study a pilot for a larger investigation of whether disparities exist across a wider spectrum of breast cancer care, including radiation therapy, hormonal therapy and chemotherapy. Together, these measures should provide a strong indicator of cancer care availability in Northern California.
 "Perhaps we shouldn’t consider it reconstruction but rehabilitation. It’s all part of the process of feeling better and moving on from the cancer."
"Perhaps we shouldn’t consider it reconstruction but rehabilitation. It’s all part of the process of feeling better and moving on from the cancer."
Although breast reconstruction is not medically necessary, other studies suggest it is a good indicator of patient outcomes. Women who receive reconstruction have improved rates of survival. While this may be due to factors such as insurance coverage or cancer stage, Martinez says it also is associated with a woman's investment in her own treatment. Patients who receive reconstruction are more likely to be involved in their care, more willing to commit to multiple surgeries, and must receive a greater degree of medical care and surveillance afterward.
"Perhaps we shouldn't consider it reconstruction but rehabilitation," Martinez says. "It's all part of the process of feeling better and moving on from the cancer." Martinez himself does not perform reconstruction surgeries, which are done by plastic surgeons.
Wendy Shadowens would certainly agree, despite the fact that breast reconstruction is a long and often painful process. While still on the operating table after her mastectomy in March 2009, Shadowens had temporary expanders – bags filled with saline solution – inserted in her chest. Their job is to gradually stretch the muscle and skin to accommodate permanent silicone implants. After about a month of healing, Shadowens began visiting her plastic surgeon every week to have more fluid added to the expanders.
"The expansion process is a pain," she says. "It hurts. You spend six months taking Vicodin." Eventually, she had an operation in which the expanders were replaced with silicone implants. A mismatch between the size of her rib cage and her implants meant that Shadowens had to undergo an additional surgery. She still has weakness in her pectoral muscles, and faces one final surgery later this summer to reconstruct her nipples. "But the end results are worth the pain you go through."
Even after the discomfort and inconvenience, Shadowens is extremely happy that she decided to have her breasts reconstructed. "If I didn't tell anyone I was a breast cancer survivor, they would never know," she says. "It's almost as if you went through a terrible car accident that hasn't left a major mark – there are no scars to show the world."


 African-American women have poorer survival rates than their white and Hispanic counterparts regardless of whether they receive radiation therapy following lumpectomy or mastectomy,
African-American women have poorer survival rates than their white and Hispanic counterparts regardless of whether they receive radiation therapy following lumpectomy or mastectomy, 




