Residency Program - Case of the Month
August 2018 - Presented by Dr. Ananya Datta Mitra (Mentored by Dr. Chihong Heidi Zhou)
Clinical History
A 24 year old homeless man presented to the UCD Medical Center with five months of progressive diarrhea which worsened in the past 2 months. According to the patient there was no inciting agent which has precipitated his diarrhea. He has watery diarrhea 4-6 bouts a day with no hematochezia (blood in stool), steatorrhea (greasy stool) or change in color of the stool; however, he does note that his diarrhea is particularly foul smelling, like "dead intestines." He also notes that the bouts of diarrhea get precipitated every time he eats which makes him avoid food. During the night he is awakened by bouts of diarrhea with occasional incontinence. When his symptoms first started, five months back, he did have some associated nausea and vomiting with abdominal cramping which has resolved since then. During this time he has lost approximately 75 pounds, has dizziness and light headedness while standing and also bilateral calf cramps intermittently. He tried over the counter anti-diarrheal medications without any effect. Of note, he is homeless since he was 10 years of age, eats food from a Food Bank and gets water from a church. He endorses smoking tobacco, as well Marijuana daily and methamphetamine 2-3 times a month but denies intravenous drug use and ethanol abuse.
He denies any history of recent travel, drinking water from river, fever, chills or cough. There is no family history of inflammatory bowel disease or cancer. No prior history of abdominal surgeries or recent hospitalizations or antibiotic use.
On physical examination, he was severely cachectic and irritable. He had a blood pressure of 100/60 mm Hg with atrial fibrillation and tachycardia (heart rate 102/min). Lungs are clear to auscultation bilaterally with no wheezing. The abdomen is soft, nontender, nondistended with normal active bowel sounds. On his skin, there are thick hyperpigmented lesions over left knuckles and right elbow. He also had an amateur tattoo on his left calf. His extremities are well perfused with no edema; he is alert and oriented with no other significant physical findings.
His labs show leukopenia (WBC: 2.8 K/cmm), normocytic anemia (Hb: 7.4g/dL; MCV: 80.5 U/MM3), electrolyte imbalance (Sodium: 134 mmol/L and potassium: 3.1 mmol/L), hypoproteinemia (albumin: 2.4g/dL). His stool examination is otherwise normal without ova and parasites; however, he had increased fecal split fats in his stool suggestive of impaired absorption of nutrients. His CD4 and CD8 counts are given in the table (Table 1) below:
Table 1: CD4 / CD8 compontent results
| Component | Value | Ref Range & Units |
| CD3+CD4+% | 2 (L) | 31 - 66 % |
| CD3+CD8+% | 67 (H) | 8 - 38 % |
| CD3% | 74 | 59 - 89 % |
| CD4/CD8 ratio | <0.1 (L) | 0.9 - 3.6 ratio |
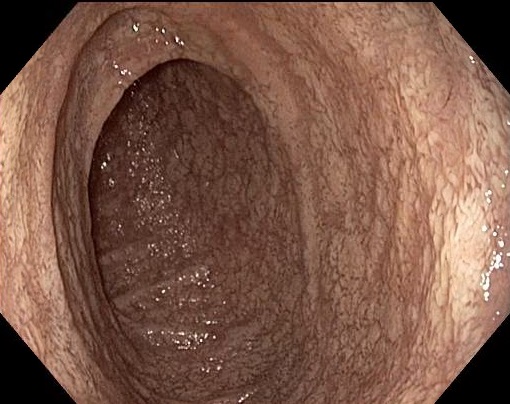
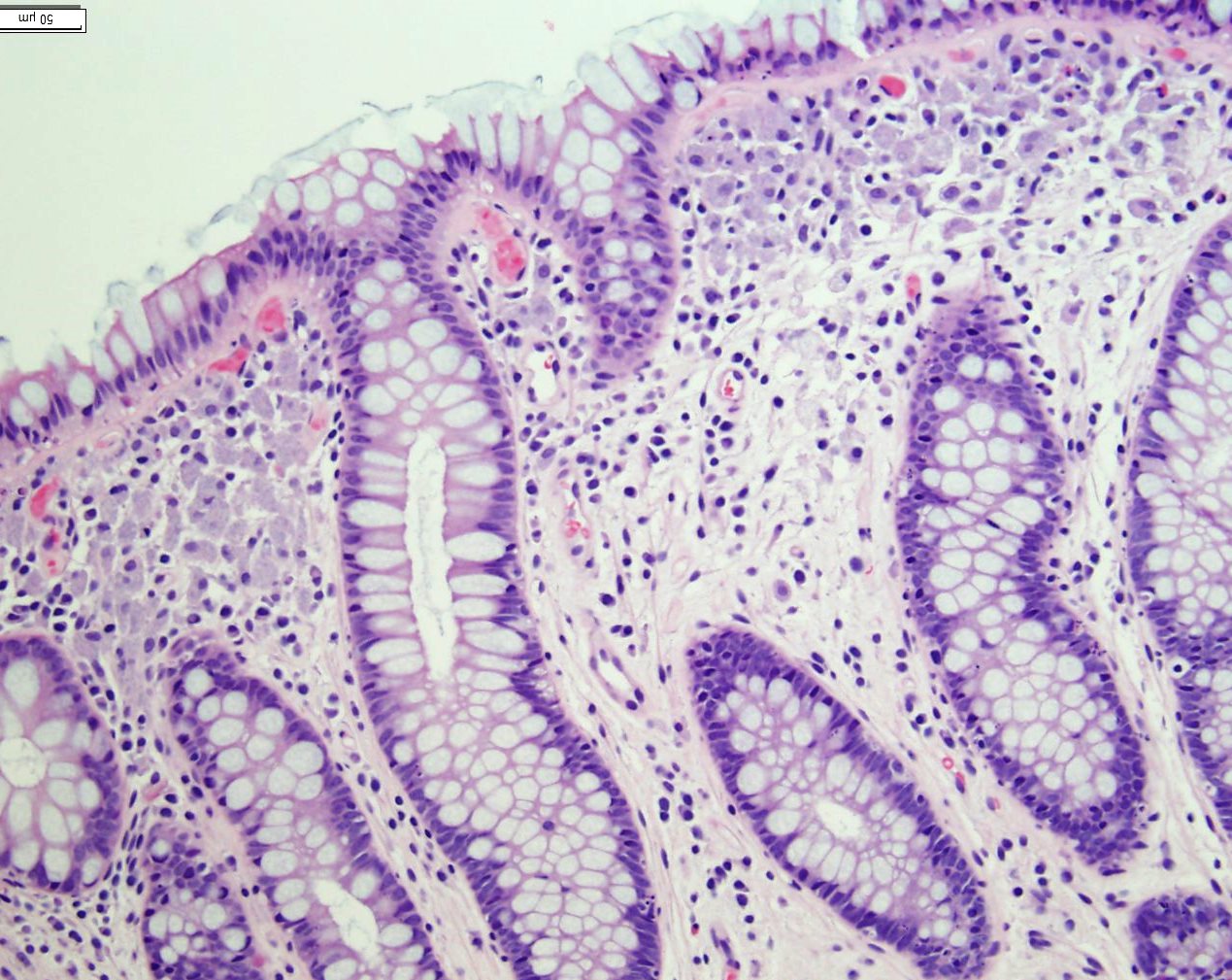
Upper GI (gastro-intestinal) endoscopy revealed patchy areas of blunted villi in 2nd portion of duodenum with whitish appearing mucosa (Figure1) and candida esophagitis (image not shown). His colonoscopy appeared normal with no evidence of neoplasia, or mucosal abnormality.
Microscopic Findings
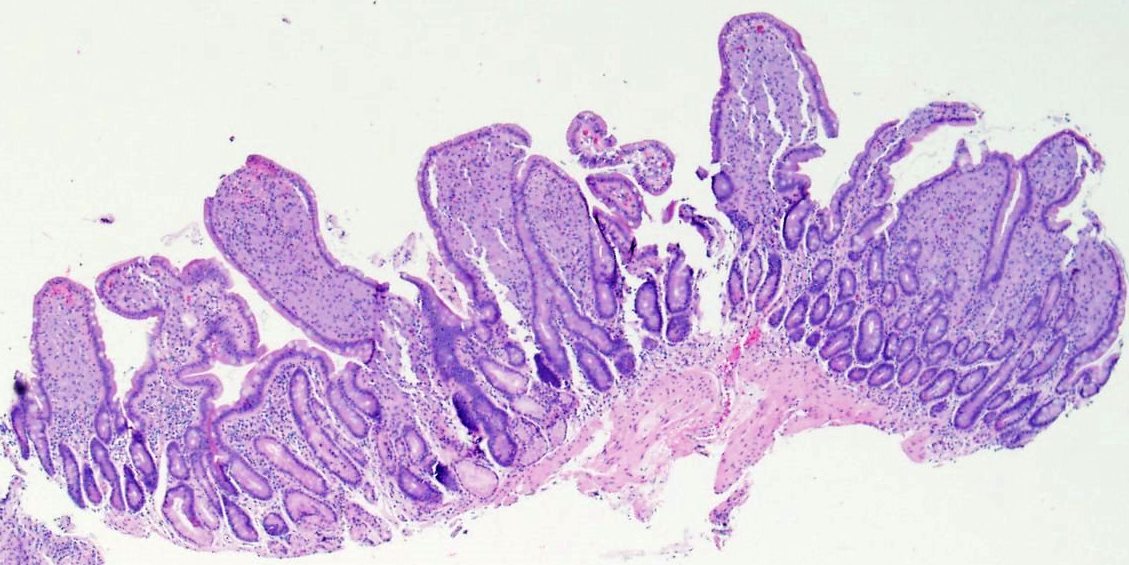
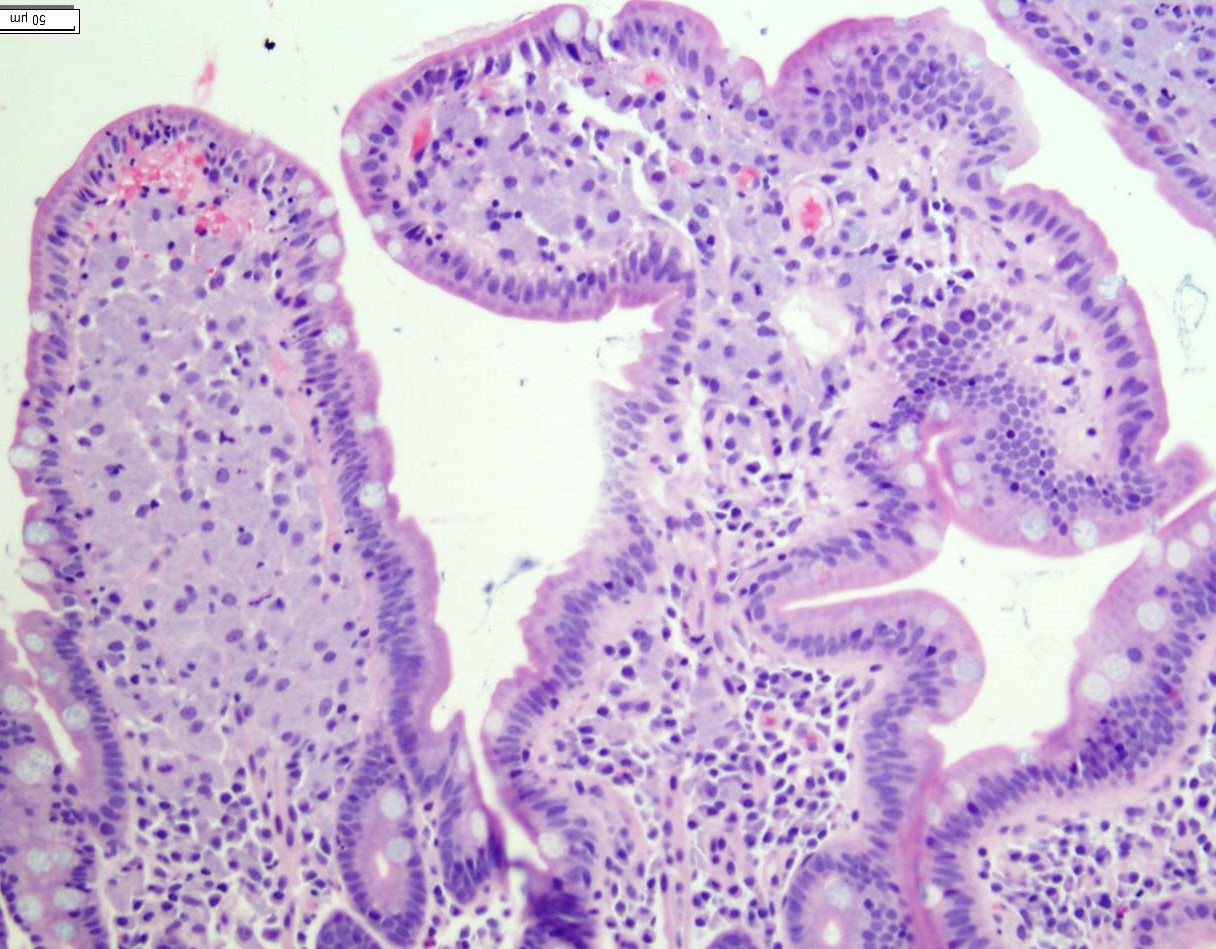
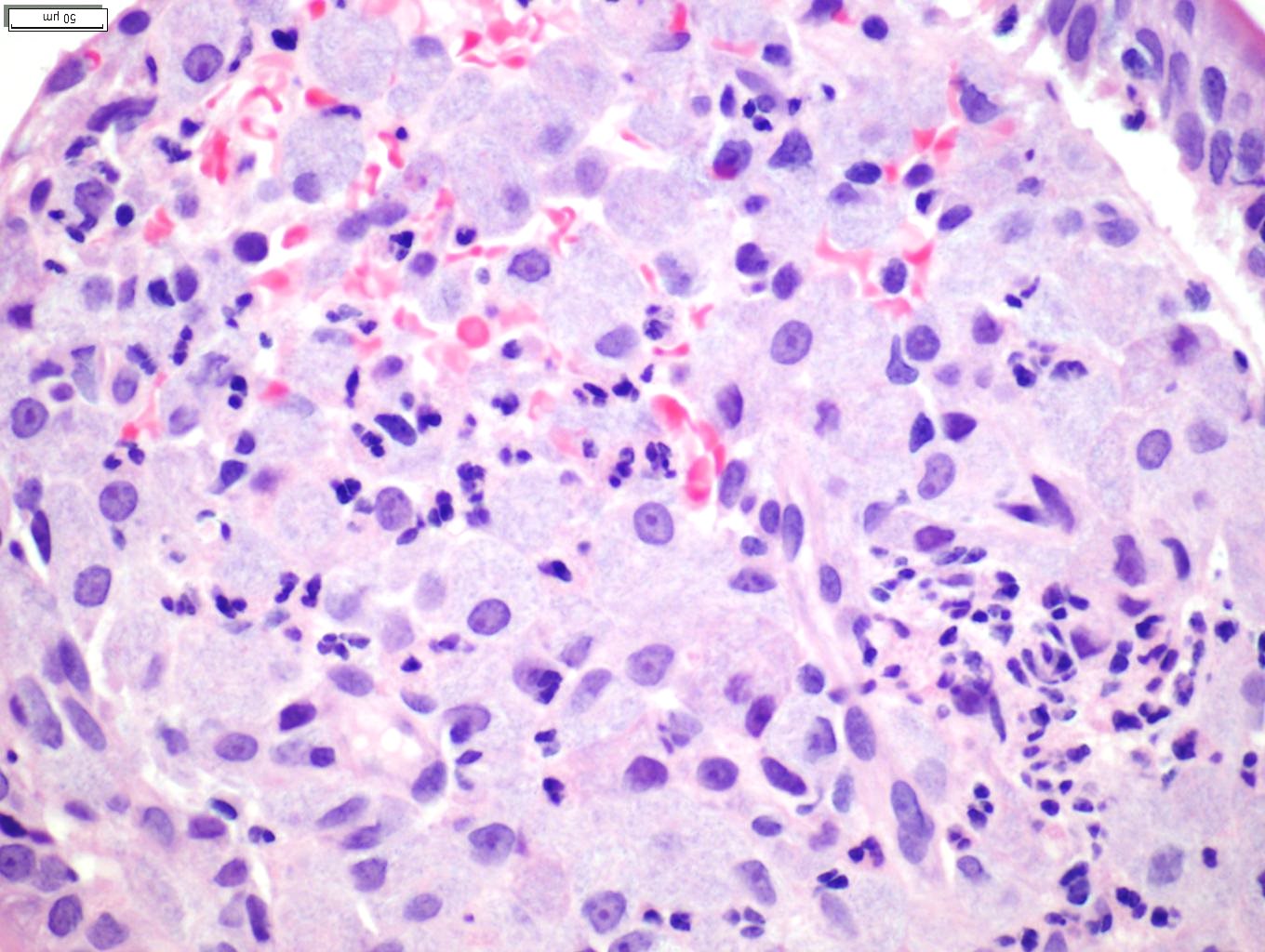
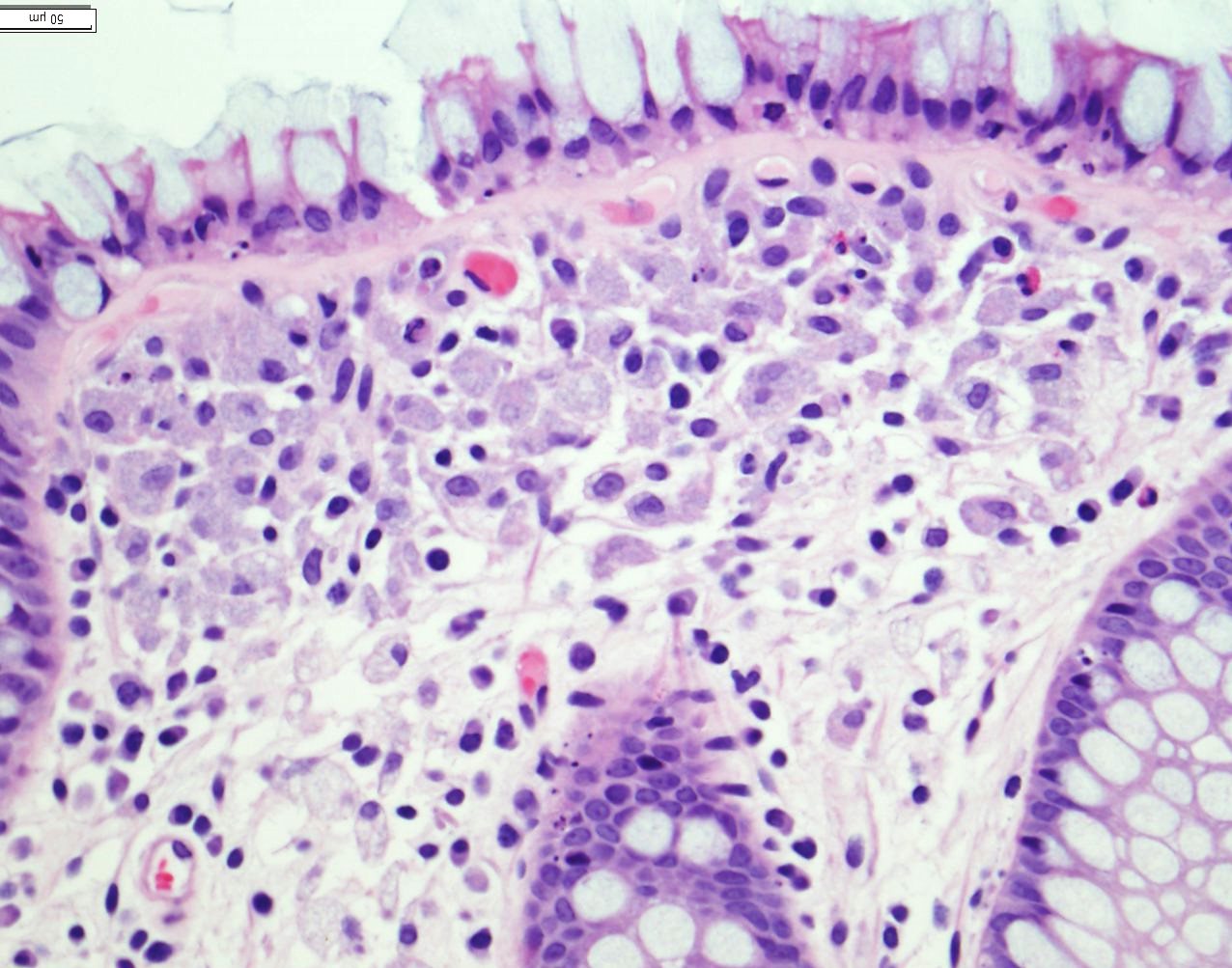
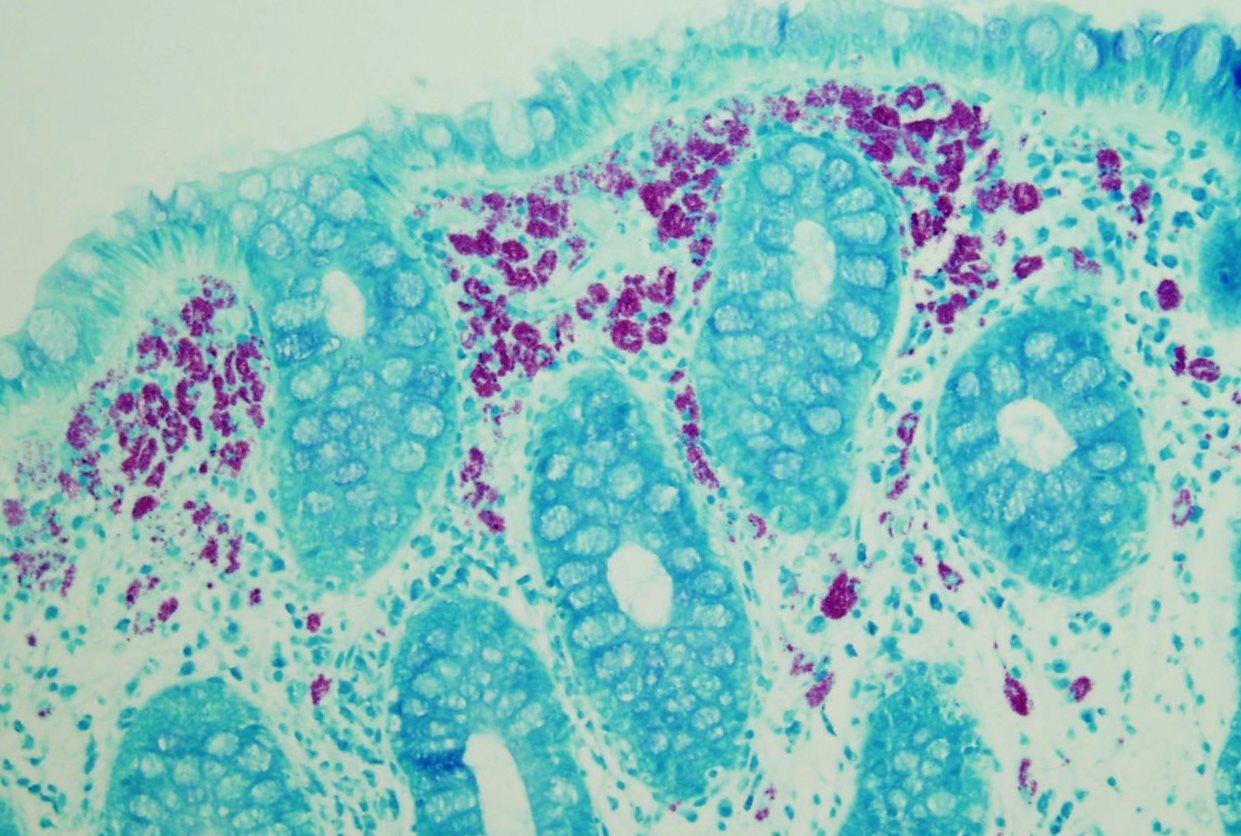
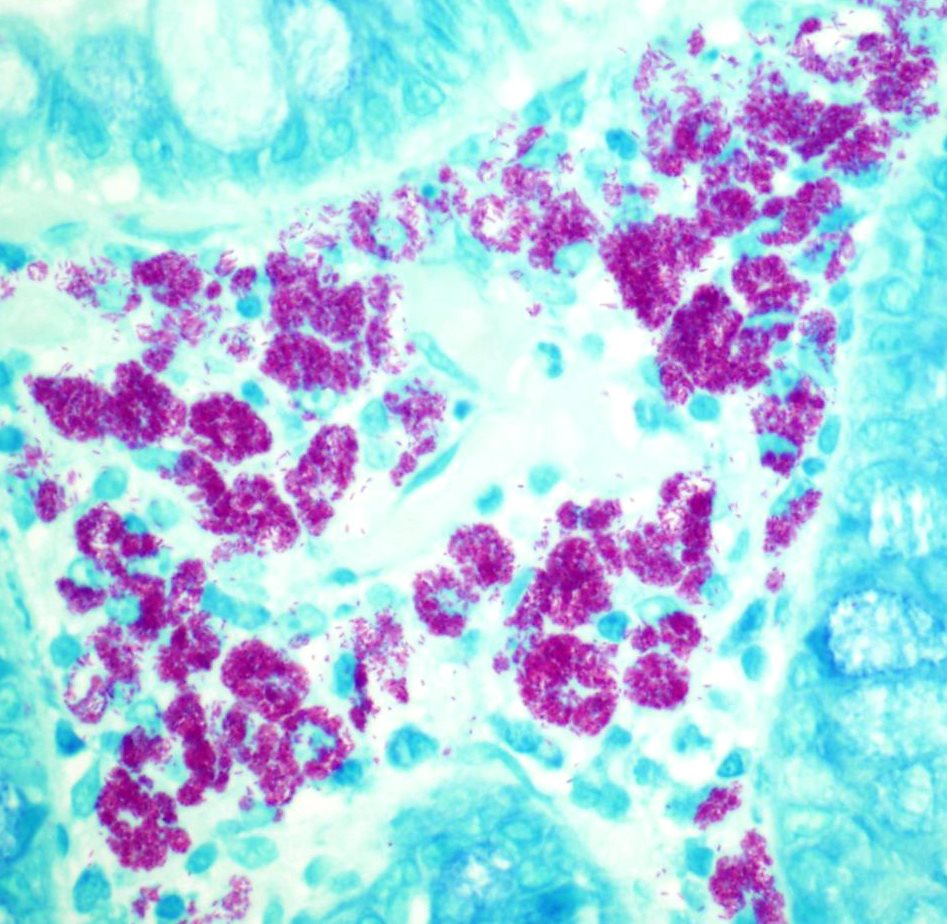
Histologically, there is evidence of Candida esophagitis (figure not shown). The second portion of the duodenum has blunted villi with expansion of the lamina propria (Figure 2-4). Lamina propria expansion with macrophages is also seen throughout his colon from terminal ileum to rectum (Figure 5-6).
Click on image to enlarge
| Figure 1 | Figure 2 | |
 |
 |
|
| Figure 3 |
Figure 4 | |
 |
 |
|
| Figure 5 | Figure 6 | |
 |
 |
Special Stains
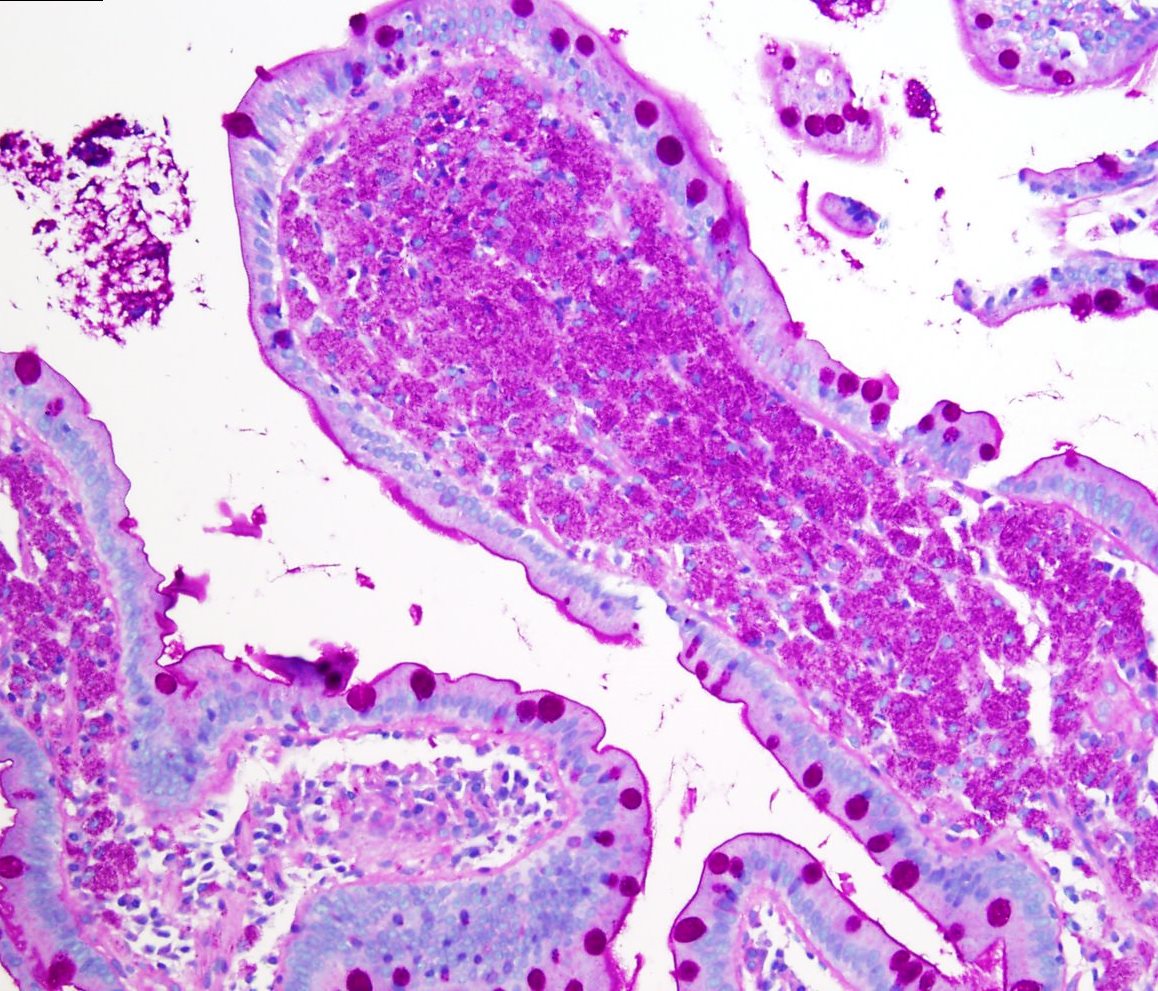
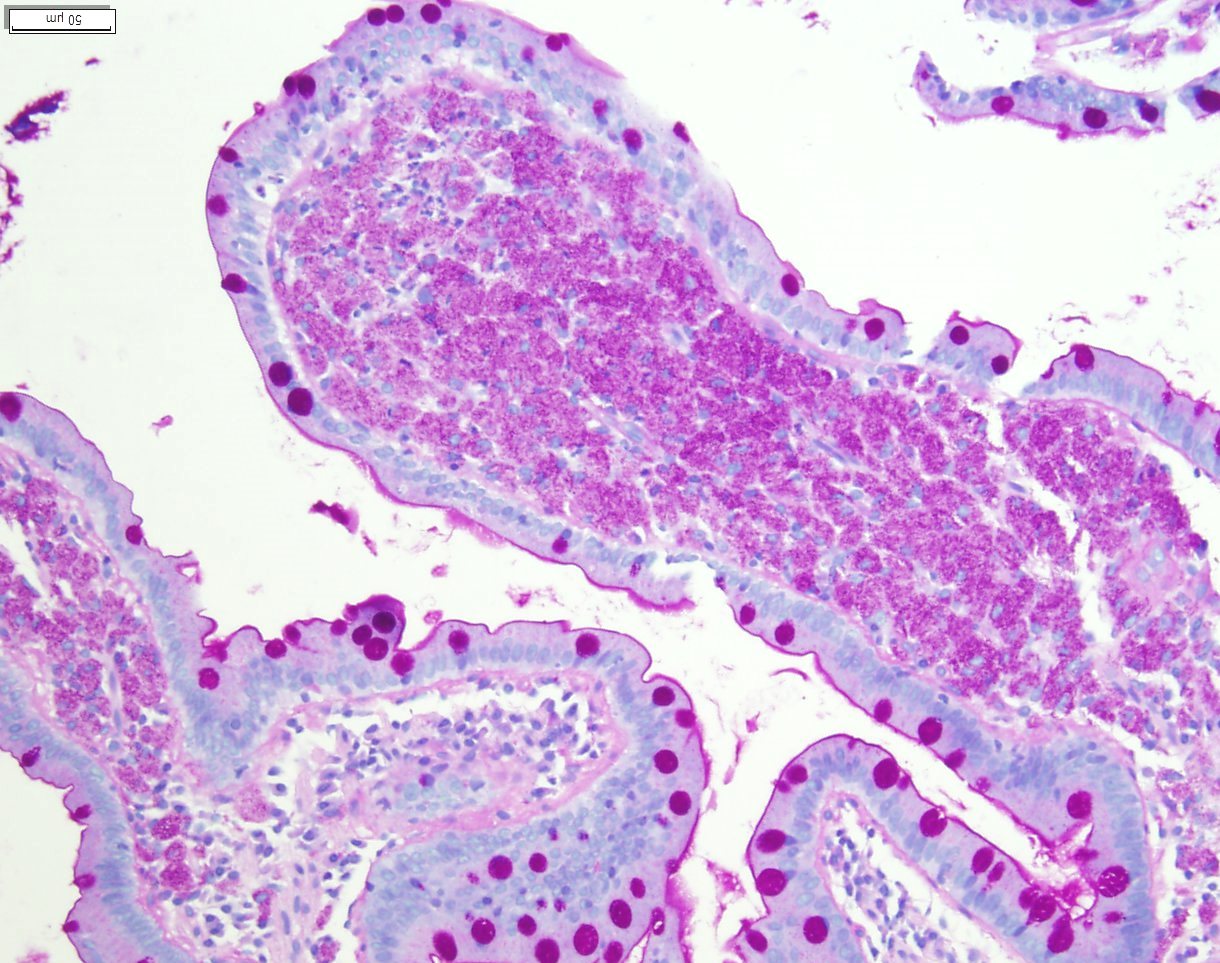
Special stains performed and interpreted at U.C. Davis Medical Center revealed the following results in the area of interest in the duodenum (Figure 7-8) and rectum (Figure 9-10):
PAS: Positive in macrophages (Figure 7)
PASD: PAS positive and diastase resistant in macrophages (Figure 8)
AFB: Positive rod like organisms in the macrophages (Figure 9-10)
Click on image to enlarge
| Figure 7 | Figure 8 | |
 |
 |
|
| Figure 9 | Figure 10 | |
 |
 |
Which of the following is most likely the diagnosis?
Choose one answer and submit.
B.) Mycobacterium avium-intracellulare (MAC) enterocolitis
> Learn more about this diagnosis.

 Meet our Residency Program Director
Meet our Residency Program Director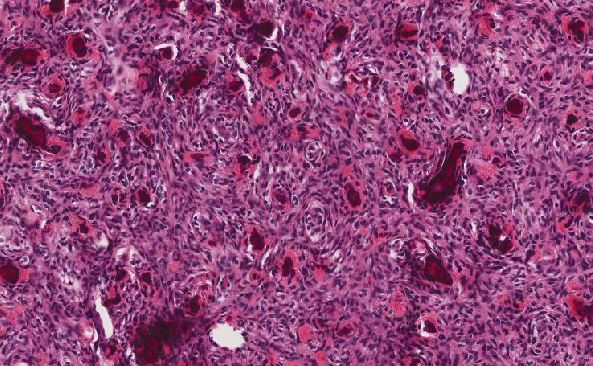
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May