Case of the Month
June 2017 - Presented by Dr. Pritesh Chaudhari & Dr. Tao Wang
Discussion
Collagenous gastritis (CG) is a rare idiopathic disorder characterized by the distinctive endoscopic-histopathologic finding of a thickened (> 10 μm) gastric subepithelial collagen layer in association with inflammatory cell infiltrate in the lamina propria. There are over 25-case reports of collagenous gastritis reported worldwide of which 10 are pediatric cases.
Although rare, the literature divides collagenous gastritis into distinct pediatric-onset and adult-onset phenotypes. The classic pattern in children centers around upper gastrointestinal symptoms including abdominal pain and severe anemia. In contrast to the adult phenotype, inflammatory changes and collagenous band deposition is usually limited to stomach and CG has a variable clinical and histopathological response to therapy. Adult type CG is linked with several autoimmune processes and celiac disease which is not seen in the childhood form. As opposed to pediatric-onset collagenous gastritis, the adult-onset form is associated with collagenous colitis and presents clinically with voluminous non-bloody diarrhea.
The etiology of collagenous gastritis is unclear; one hypothesis is a vascular abnormality with increased vascular permeability resulting in deposition of extruded protein and collagen deposition. Alternatively a primary inflammatory process results in a secondary fibrotic scarring process in susceptible individuals.
Treatment of CG in either age group remains poorly defined; treatment strategies have revolved around the etiopathologic observations suggesting an inflammatory process and the association with celiac disease. Both anti-inflammatory and anti-secretory measures as well as gluten free diet have been tried but there has been, to date, no comprehensive review of treatment strategies and outcomes in this population.
In conclusion, collagenous gastritis in children tends to be an isolated process that follows a generally benign course with limited long-term morbidity and no increased mortality reported to date. Clinical investigation in children with collagenous gastritis needs to include investigation for H. Pylori and colonoscopy to rule out collagenous colitis.
References
- Abdo AA, Zetler PJ, Halparin LS: Familial microscopic colitis. Can J Gastroenterol 2001, 15:341-343.
- Hijaz, Nadia Mazen et al. “Clinical Outcome of Pediatric Collagenous Gastritis: Case Series and Review of Literature.” World Journal of Gastroenterology : WJG 19.9 (2013): 1478–1484. PMC. Web. 9 June 2017.
- Cote JF, Hankard GF, Faure C et al.: Collagenous gastritis revealed by severe anemia in a child. Hum Pathol 1998, 29:883-886.
- Suskind, David et al. “Collagenous Gastritis, a New Spectrum of Disease in Pediatric Patients: Two Case Reports.” Cases Journal 2 (2009): 7511. PMC. Web. 9 June 2017.
- Lagorce-Pages C, Fabiani B, Bouvier R et al.: Collagenous gastritis: a report of six cases. Am J Surg Pathol 2001, 25:1174-1179.
- Meunier S, Villard F, Bouvier R et al.: Collagen gastritis, an unusual cause of anemia in children. Report of 2 cases. Arch Pediatr 2001, 8:47-50.
- Park S, Kim DH, Choe YH et al.: Collagenous gastritis in a Korean child: a case report. J Korean Med Sci 2005, 20:146-149.

 Meet our Residency Program Director
Meet our Residency Program Director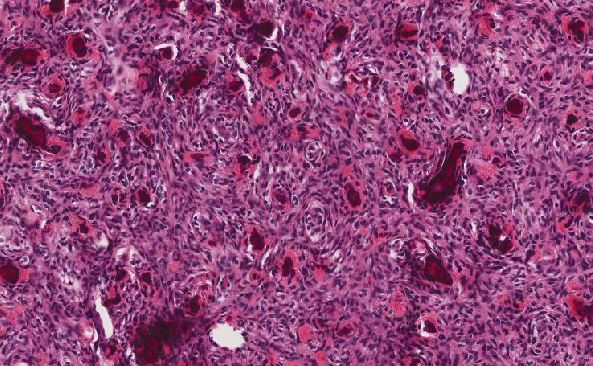
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May