Case of the Month
November 2015 - Presented by Dr. Adam Stelling
Answer:
d. Hemolytic Uremic Syndrome
Discussion:
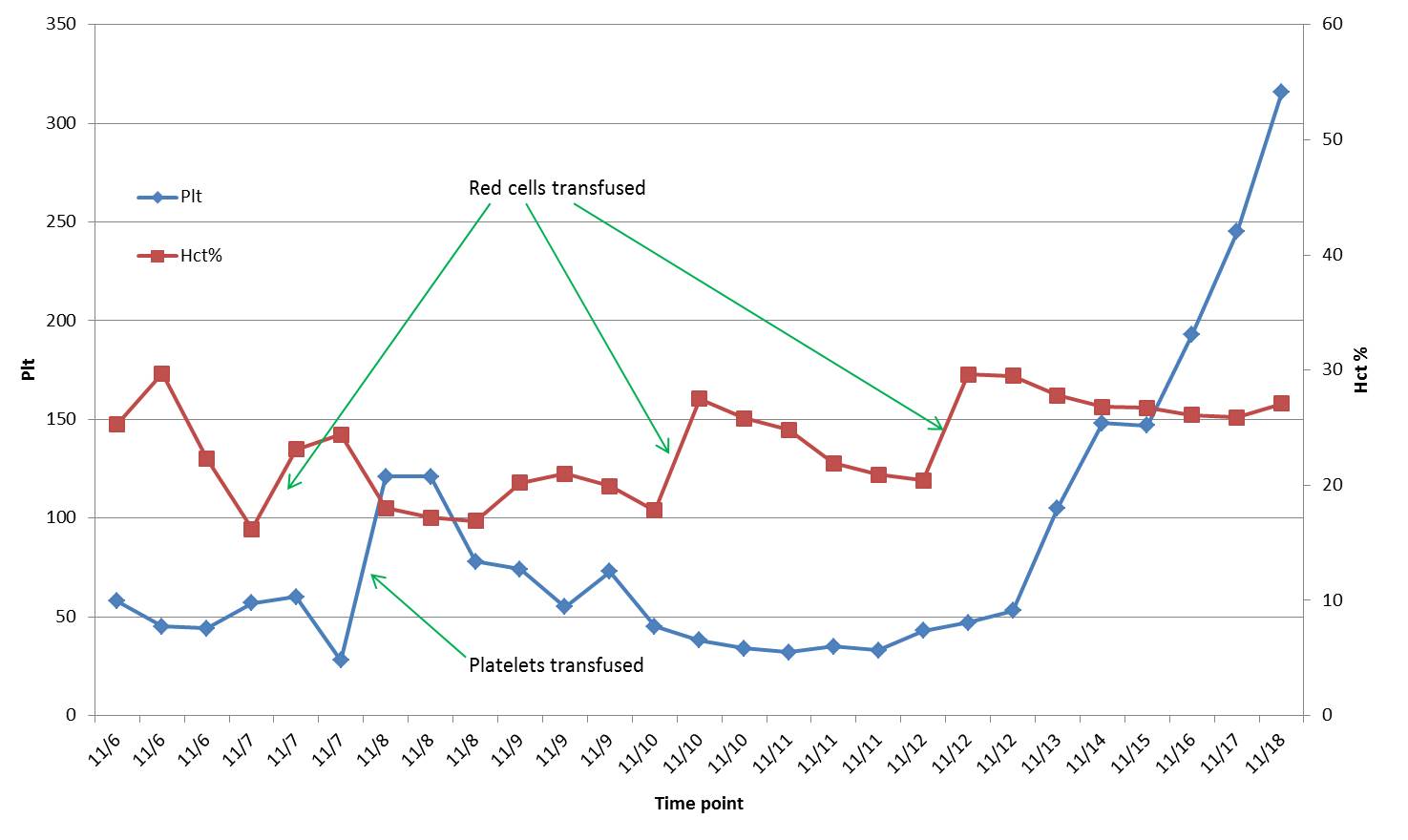
This patient has Hemolytic Uremic Syndrome and exhibits the classic triad of findings with microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Typically seen in children, it is one of the most common causes of pediatric kidney injury. One of the initial laboratory findings and a hallmark of this disease is the presence of schistocytes, or fragmented red blood cells, in the peripheral blood. The differential diagnosis of schistocytes includes microangiopathic hemolytic anemias such as Hemolytic Uremic Syndrome (HUS), Thrombotic Thrombocytopenic Purpura (TTP), Disseminated Intravascular Coagulation (DIC), and some systemic autoimmune diseases. A normal INR and aPTT is important to rule out a consumptive coagulopathy from DIC secondary to other causes. In this case, the diagnosis of HUS is strongly supported by the age of the patient, symptoms of a lower GI infection with bloody diarrhea, and presence of shiga toxin-producing E. coli. Approximately 90% of HUS cases are due to shiga toxin-producing E. coli infections and lead to microangiopathic hemolytic anemia through toxin mediated endothelial damage of small vessels, especially in the kidneys. A less commonly, Streptococcus pneumoniae infections can cause HUS. These cases require special considerations from the blood bank as bacterial neuraminidase removes red cell surface glycoproteins to uncover occult antigens known as “T” antigens. T-antibodies exist as a naturally occurring IgM with variable titers in individual plasma and may induce hemolysis through complement activation. Red cells for transfusion will be washed in order to remove any T-antibody in the residual donor plasma. If plasma containing products are needed, a minor crossmatch may be performed using donor plasma to rule out T-antigen activation. The very rare cases of primary, or atypical, HUS may be caused by mutations in or inhibitors to complement regulatory proteins including C3, factor H, factor B, and factor I. A recent FDA approval for a terminal complement inhibitor called Eculizumab can control the disease. In contrast, cases of infectious associated HUS can be treated supportively with antibiotics, hydration, and transfusion. Improvements in platelet counts, as is seen in our patient, are a sign of recovery and the resolution of vascular injury.

 Meet our Residency Program Director
Meet our Residency Program Director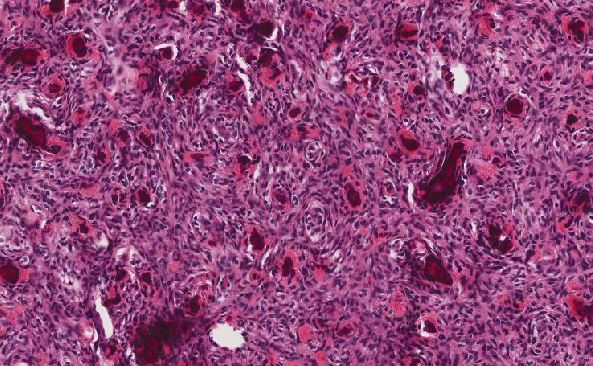
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May