Case of the Month
October 2015 - Presented by Dr. Nima Amini
Answer:
D) Spitzoid melanoma of childhood
Discussion:
What are some of the histologic differences between Spitzoid melanoma of childhood and spitzoid nevus? What is the best indication to distinguish spitzoid melanoma of childhood from spitz nevus and atypical spitz tumor?
Although both entities are composed of melanocytic nests, histologically the spitzoid melanoma is bigger in size, it’s nests are also bigger with higher melanocytic mitotic rates, the bigger nests can be seen deeper in the dermis (unlike spitz nevus that nests get smaller at the deeper boarders of the nevus) and tumor cells have larger nucleoli and nuclei (Figure 1), comparing to a spitz nevus. Lymph nodes involved by sheets of tumor cells with cytogenetic features of a typical melanoma is the best indication to distinguish this entity from spitz nevus and atypical spitz tumor. ³
What are histologic differences between spitzoid melanoma of childhood and conventional melanoma in low power?
Spitzoid melanoma of childhood does not have a macular stage and often grows fast.1,2 Spitzoid melanoma of childhood is usually growing vertically; hence, it has a higher mean thickness comparing to conventional melanoma. In some cases spitzoid melanomas are symmetric in contrast to conventional melanoma which is often asymmetric. Spitzoid melanoma of childhood is usually sharply circumscribed with nests that are present at the end of the lesion and sometimes does not have a remarkable intra-epidermal component.³
What are some of the cytogenetic features of the spitzoid melanoma of childhood?
Based on FISH studies, specific risk categories of spitzoid melanocytic neoplasms in children are identified (Gerami et al, 2013); Homozygous 9p21 deletions has the highest risk for aggressive behavior while isolated 6q23 deletions or no copy number aberrations carry less risk for such behavior.4 Immunohistochemical staining for p16 in our case showed only partial loss of expression within the tumor, suggesting that biallelic loss of chromosome 9p is unlikely, possibly a favorable prognostic indicator in this context.
What are the prognosis and survival rate in different age groups?
According to a study performed by Pol-Rodriquez et al, comparing two age groups (0-10 and 11-17), The younger age group (as in our case) had a higher rate of local metastasis (86%) and 14% distant metastasis; while the older age group had more distant metastasis (41%) and patients in younger age group had a better survival rate.
What key features should be identified in a melanoma pathology report in general?
According to Rapini, the key elements that should be part of any melanoma pathology report include: Histologic subtype (SSM, LM, NM, ALM…etc), Breslow thickness (the most important feature, thickness from the top of the granular layer to the deepest tumor invasion), mitotic rate (mitotic figures counted per square millimeter), presence of ulcer (usually at the center of the tumor which means the lesion is more active and proliferative), horizontal or vertical growth, tumor regression (The area of previous tumor removed by the immune system), angio-lymphatic and peri-neural involvement, microsatellitosis, tumor infiltrating lymphocytes, cytologic type (epithelioid, spindle, or small cell), nevus association (if any) and surgical margins.5
References:
- Roaten JB, Partrick DA, Bensard D. Survival in sentinel lymph node positive pediatric melanoma. J Pediatric Surg. 2005; 40(6):988-992; discussion 992
- Pol-Rodriquez M, Lee S, Silvers DN.Influence of age on survival in childhood spitzoid melanomas. Cancer. 2007; 109(8): 1579-1583
- Guido Massi, Philip E Leboit. Histologic diagnosis of nevi and melanoma. 2nd edition. 2014; 501-510
- Gerami P, Cooper C, Bajaj S, Wagner A, Fullen D, Busam K, Scolyer R, Xu X, Elder D, Abraham R, Prieto V, Guitart J, Liu P, Pestova E, Barnhill R. Outcomes of Atypical Spitz Tumors With Chromosomal Copy Number Aberrations and Conventional Melanomas in Children. (Am J Surg Pathol 2013;37:1387–1394)
- Rapini R. Practical Dermatopathology.2nd edition. 2012; 305

 Meet our Residency Program Director
Meet our Residency Program Director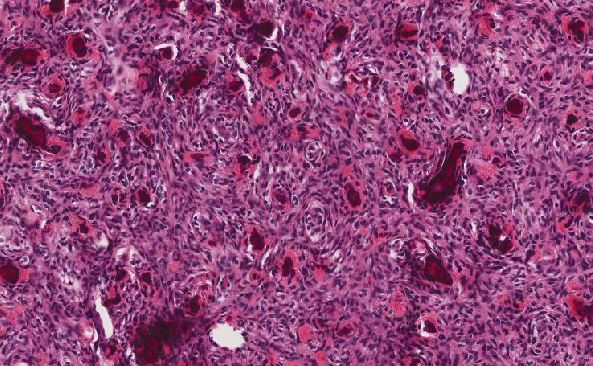
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May