Residency Program - Case of the Month
January 2015 - Presented by Dr. Nicholas Coley & Dr. Gloria Lewis, Mather Veteran Affairs
Answer:
Hyalinizing trabecular adenoma
Discussion:
Hyalinizing trabecular adenoma (HTA) is a rare and disputed thyroid lesion most prevalent in women aged 40-60. The entity was first described in 1987 by Carney et al. as a neoplasm consisting of a trabecular growth pattern of cells within a hyalinizing stroma and/or abundant amounts of hyalinized cytoplasm. Most pathologists regarded the entity as a benign neoplasm while others argue it is a variant of papillary thyroid carcinoma (PTC).
Those favoring HTA as a variant of PTA pointed out that morphologically both entities feature hypercellularity and nuclear grooving, pseudoinclusions, and nuclear hyperchromaticity (Gupta et al., 2010; Bishop and Ali, 2011; Kim et al., 2011; Santosh et al., 2011). Additionally, proponents of HTA as a variant of PTC argued both lesions share similar genetic alterations as both HTA and PTC contain RET/PTC gene rearrangements assayed by reverse transcription-polymerase chain reaction and immunohistochemistry at nearly identical frequencies (Cheung et al., 2000; Papotti et al., 2000).
Proponents who endorse HTA as a distinct entity from PTC point out that PTC often displays strong staining for CK19 and galectin-3 whereas HTA weakly expresses both markers (Salvatore et al., 2005). Furthermore, HTA exhibits unique membrane staining for MIB-1 absent in PTC (Leonardo et al., 2007). Molecularly, PTC displays frequent lesions in the BRAF and N-ras genes not detected in HTA to date (Salvatore et al., 2005), and the five microRNAs upregulated in PTC are downregulated in HTA (Sheu et al., 2010). The prognosis of HTA is very favorable and treatment via lobectomy or hemithyroidectomy is curative. In a study of 119 cases of diagnosed HTA followed for a median of 10 years, 118 displayed no aggressive behavior (capsular, vascular, and/or parenchymal invasion) while a sole case progressed to vascular and capsular invasion with lung metastasis. If a neoplasm containing histology consistent with a HTA invades the capsule, it is considered a hyalinizing trabecular carcinoma (an entity for which even less data exists). Thus, owing to the aforementioned molecular evidence and the extremely favorable clinical outcome, HTA is currently diagnosed as a benign neoplasm as opposed to a PTC variant.
Surgeons should be educated that HTA is frequently misdiagnosed as PTC particularly on frozen section or cytology using fine needle aspiration where the trabecular architecture and hyalinized stroma are frequently distorted or not present in HTA (Casey et al., 2004). Currently the etiology of HTA has yet to be clarified. HTA frequently arises in the background of chronic lymphocytic thyroiditis or in association with PTC (both observed in our patient), but it is unknown if or how these processes are causally related to HTA.
In Summary:
- HTA can be a pitfall for PTC on FNA due to the presence of intranuclear pseudoinclusions; however, features of HTA which can distinguish it from PTC include: vague palisading architecture, extracellular metachromatic material (hyaline), follicular cells with nuclear atypia of PTC with filamentous cytoplasm. However, PTC is relatively common while HTA is extremely rare and most FNA showing intranuclear pseudoinclusions are in fact PTC.
- Most pathologists currently regard HTA as a benign entity because of its excellent prognosis. The lesion almost never metastasizes and is cured if completely excised.
Sources Cited:
Bishop JA and Ali SZ: Hyalinizing trabecular adenoma of the thyroid gland. Diagn Cytopathol 39: 306-310, 2011.
Casey MB, Sebo TJ and Carney JA: Hyalinizing trabecular adenoma of the thyroid gland: cytologic features in 29 cases. Am J Surg Pathol 28: 859-867, 2004.
Cheung CC, Boerner SL, MacMillan CM, Ramyar L and Asa SL: Hyalinizing trabecular tumor of the thyroid: a variant of papillary carcinoma proved by molecular genetics. Am J Surg Pathol 24: 1622-1626, 2000.
Gupta S, Modi S, Gupta V and Marwah N: Hyalinizing trabecular tumor of the thyroid gland. J Cytol 27: 63-65, 2010.
Kim T, Oh YL, Kim KM and Shin JH: Diagnostic dilemmas of hyalinizing trabecular tumours on fine needle aspiration cytology: a study of seven cases with BRAF mutation analysis. Cytopathology 22: 407-413, 2011.
Leonardo E, Volante M, Barbareschi M, Cavazza A, Dei Tos AP, Bussolati G and Papotti M: Cell membrane reactivity of MIB-1 antibody to Ki67 in human tumors: fact or artifact? Appl Immunohistochem Mol Morphol 15: 220-223, 2007.
Papotti M, Volante M, Giuliano A, Fassina A, Fusco A, Bussolati G, Santoro M and Chiappetta G: RET/PTC activation in hyalinizing trabecular tumors of the thyroid. Am J Surg Pathol 24: 1615-1621, 2000.
Salvatore G, Chiappetta G, Nikiforov YE, Decaussin-Petrucci M, Fusco A, Carney JA and Santoro M: Molecular profile of hyalinizing trabecular tumours of the thyroid: high prevalence of RET/PTC rearrangements and absence of B-raf and N-ras point mutations. Eur J Cancer 41: 816-821, 2005.
Santosh KV, Raychaudhuri S, Subramanya H and Naveen Kumar BJ: Cytology of hyalinising trabecular adenoma-like variant of medullary thyroid carcinoma. J Cancer Res Ther 7: 189 191, 2011.
Sheu SY, Vogel E, Worm K, Grabellus F, Schwertheim S and Schmid KW: Hyalinizing trabecular tumour of the thyroid – differential expression of distinct miRNAs compared with papillary thyroid carcinoma. Histopathology 56: 632 640, 2010.

 Meet our Residency Program Director
Meet our Residency Program Director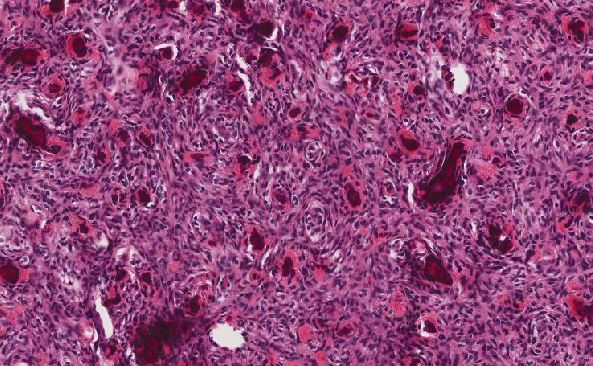
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May