Residency Program - Case of the Month
April 2014 - Presented by Saba Ali, M.D.
Answer:
Malignant mixed germ cell tumor
Figure 1: Mature teratoma (colon adenocarcinoma)
Figure 2: Mature teratoma with benign colonic mucosa (left) and colonic adenocarcinoma (right)
Figure 3: Choriocarcinoma
Figure 4: Yolk sac tumor with intermixed embryonal carcinoma
Microscopic Description:
Mixed germ cell tumors arise from the primordial germ cells located in the developing gonads. The various morphological patterns of germ cell tumors fall under the category of germinomatous or dysgerminomatous. Dysgerminomatous germ cell tumors comprise extraembryonic re yolk sac and placenta, and embryonic differentiation. Subtypes include embryonal carcinoma, yolk sac tumor (extraembryonic), choriocarcinoma (extraembryonic), teratoma (immature and/or mature), polyembryoma and gonadoblastoma. Mixed germ cell tumors include both categories, and may be benign or malignant.
Malignant mixed germ cell tumors comprise <10% of all malignant ovarian germ cell tumors. The majority of tumors arise in women of reproductive age (<30 years), and clinical presentation varies from nonspecific abdominopelvic pain and fullness to vaginal bleeding. Physical examination of a unilateral or bilateral mass and imaging techniques are important for clinical diagnosis. Tumor markers are also used to help direct the diagnosis, and the marker subtype is dependent on the tumor component-alpha fetoprotein (yolk sac tumor), human chorionic gonadotropin (choriocarcinoma), lactate dehydrogenase (embryonal carcinoma). The tumor can grow to occupy a large volume of the body cavity, and is prone to hemorrhage, torsion, and rupture. Diagnostic confirmation is via surgery.
Grossly, mixed germ cell tumors can grow up to 15 cm in diameter. The external surfaces may be smooth and glistening, or irregular and rough. The appearance of the cut surfaces relies on the type of tumor. Choriocarcinomas manifest as solid tumors with focal areas of hemorrhage and necrosis, while embryonal carcinomas are yellow-gray and are usually without cystic lesions. Yolk sac tumors are friable and bosselated, with gray-yellow surfaces and ample areas of cystic degeneration, hemorrhage, and necrosis. Mature teratomas macroscopically correlate with the structure of differentiation re tooth, hair, or intestine. This case consisted of a mature colorectal adenocarcinoma (mature teratoma) as the major component, and embryonal carcinoma, yolk sac tumor, and choriocarcinoma as minor components.
The histological pattern is variable, and identifying all tumor components is largely dependent on adequate sampling and evaluation on gross examination. The components may be separate, adjacent to one another, or may be admixed within the same microscopic focus. Often times, immunohistochemistry staining is used to confirm what is suspected on H&E stains. Yolk sac tumors histologically have several distinct patterns, and this case in particular exhibited cribriform endodermal spaces lined by flatted cuboidal cells with intermixed areas of embryonic carcinoma. Immunohistochemically, yolk sac tumors stain negative for epithelial membrane antigen and CK 7, and are only focally positive for Leu-M1 in 60% of cases. Embryonal carcinomas are composed of sheets of ill-defined polyhedral tumor cells, with pleomorphic nuclei, vesicular chromatin, and are altogether without any architectural structure. IHC staining includes reactivity to CD 30, OCT ¾, and AE1/AE3. Choriocarcinomas resemble placental tissue. These tumors are composed of two types of cells, synctiotrophoblasts and cytotrophoblasts. Syncitiotrophoblasts are characterized by large and irregular cells, with hyperchromatic pleomorphic nuclei and abundant and often vacuolated cytoplasm. Cytotrophoblasts, which need to be present to confirm the diagnosis albeit not necessarily in the same microscopic focus, consist of small round cells with well-defined borders and nuclei which may be large or small, with prominent nucleoli. Choriocarcinomas stain positive for IHC markers cytokeratin, CD10, human placental lactogen, and epithelial membrane antigen, and negative for CD 31 and CD 34.
Resources:
- M Koshy, MBBS, MRad,*,1 A Vijayananthan, MBBS, MRad,1 and V Vadiveloo, MBBS, MOG2. Malignant ovarian mixed germ cell tumour: a rare combination. Biomed Imaging Interv J. 2005 Oct-Dec; 1(2): e10.
- Robboy. Pathology of the Female Reproductive Tract second edition. 2009
- Talerman A. Germ cell tumours. Ann Pathol. 1985;5(3):145-57.
- Leena Varughese, M.D. , Rajit Malliah, M.D. Ovary tumor, Germ cell tumors, General . PathologyOutlines.com, Inc. (c) 2002-2013

 Meet our Residency Program Director
Meet our Residency Program Director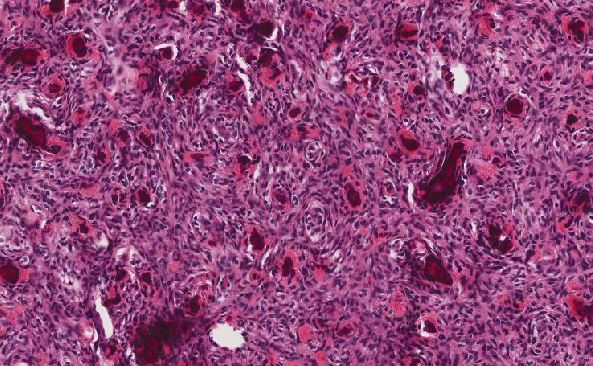
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May