Residency Program - Case of the Month
September 2012 - Presented by Rebecca Sonu, M.D.
Answer:
Uterine Carcinosarcoma (Malignant mixed müllerian tumor)
Discussion:
Carcinosarcomas of the uterus are rare and aggressive malignancies consisting of both epithelial (carcinoma) and mesenchymal (sarcoma) tumor components with malignant histology. Carcinosarcoma accounts for 2-5% of all malignancies of the uterine corpus. It is most common in postmenopausal women (median age of 66 years) but can also occur in younger women and children. The most common presentation is abnormal vaginal bleeding, bloody or watery discharge, abdominal pain or a mass.
Carcinosarcoma may develop in patients with a history of prior pelvic irradiation or those that are status post-treatment for cervical carcinoma. An association with long-term tamoxifen treatment for breast cancer has been reported, however, there is no conclusive evidence of tamoxifen having either a direct carcinogenic effect or involved role in the tumorigenesis of carcinosarcoma.1
Grossly, the tumor will typically form a broad-based polyp that fills and expands the uterine cavity often protruding through the cervix (Figures 1-3). However, these tumors can also sometimes arise from atrophic uteri. The cut surfaces may show necrosis, hemorrhage or contain gritty areas representing heterologous elements such as bone or cartilage. Microscopically, both epithelial and mesenchymal elements are malignant. The carcinomatous component, corresponding to the müllerian type, is most often a poorly differentiated serous carcinoma. Squamous elements are also frequently seen (Figure 6). Other epithelial patterns include: mucinous carcinoma, clear cell carcinoma or undifferentiated carcinoma. The stromal element may be homologous or heterologous. The homologous carcinosarcoma contains a mesenchymal element that is composed of cell types that are normally found in the uterus such as stromal sarcoma, fibrosarcoma, leiomyosarcoma or a mixture. The heterologous elements include rhabdomyosarcoma, chondrosarcoma, osteosarcoma and liposarcoma (in decreasing order of frequency).1
In this case, the tumor consisted of an endometrioid adenocarcinoma with squamous differentiation as the epithelial component and approximately 10% of a sarcomatous component with a heterologous focus of malignant osteoid.
The differential diagnosis should include the monophasic tumors of undifferentiated carcinomas and sarcomas. Keratin stains are not helpful when trying to distinguish whether an undifferentiated component is carcinoma or sarcoma because sarcomatous elements in carcinosarcoma may be composed of keratin positive cells.2 Adenosarcomas can be distinguished by well-differentiated epithelium with the characteristic mesenchymal cuffing around the glands. Low-grade endometrioid carcinomas may have foci of spindle cells which must also be considered in the differential. In carcinosarcoma, the mesenchymal component is usually high-grade with obvious anaplasia.1
Clinical and molecular studies suggest that uterine carcinosarcomas are clonal malignancies that originate from a common epithelial origin.3 Studies by Taylor et al have demonstrated this by showing that defective DNA mismatch repair and/or TP53 defects were common to both epithelial and mesenchymal components of carcinosarcomas. They proposed a model for the histogenesis of uterine carcinosarcoma in which a normal progenitor cell may acquire a number of genetic mutations (including defects in TP53 and DNA mismatch repair). As the tumor differentiates into carcinoma and sarcomatous components additional defects are acquired. Molecular defects acquired later in histogenesis will then be discordant between the two components. Additional theories include the “collision” theory, which suggests that epithelial and mesenchymal elements have arisen independently and collided. The “conversion’ theory suggests that the sarcomatous element derives from the carcinoma during the tumor’s evolution.
Evidence shows that the uterine carcinosarcomas are in reality ‘metaplastic’ carcinomas or carcinomas with sarcomatous ‘metaplasia’ with the epithelial component being the main driving force. The epithelial component is the most critical prognostic element. Survival tends to be worse for patients with a non-endometrioid epithelial component compared with an endometrioid epithelial component (5 year survival: 26% and 55% respectively).3 In addition, the epithelial component will be involved in the majority of vascular invasion and metastasis. The type of heterologous element has not been shown to be clinically useful.
Uterine carcinosarcoma are treated as high-risk endometrial carcinomas. Surgical treatment consists of total abdominal hysterectomy with staging. Responses to present-day adjuvant radiotherapy and chemotherapy are poor. The most promising treatment includes adjuvant combined chemotherapy when compared to single-agent chemotherapy or radiotherapy.3 The overall survival at 5 years for patients with uterine carcinosarcoma is only 31% compared to 84% for patients with cancer of the uterine corpus.1
References:
-
Robboy SL, Mutter GL, Prat J, et al. Robboy’s Pathology of the Female Reproductive Tract. Churchill Livingstone. 2009, 443-449.
-
Kempson RL and Hendrickson MR. Smooth muscle, endometrial stromal, and mixed mullerian tumors of the uterus. Mod Pathol. 2000;13(3):328-342.
-
de Jong R, Nijman HW, Wijbrandi TF, et al. Molecular markers and clinical behavior of uterine carcinosarcomas: focus on the epithelial tumor component. Mod Pathol. 2011;24:1368-1379.
-
Taylor NP, Zighelboim I, Huettner PC, et al. DNA mismatch repair and TP53 defects are early events in uterine carcinosarcoma tumorigenesis. Mod Pathol. 2006;19:1333-1338.

 Meet our Residency Program Director
Meet our Residency Program Director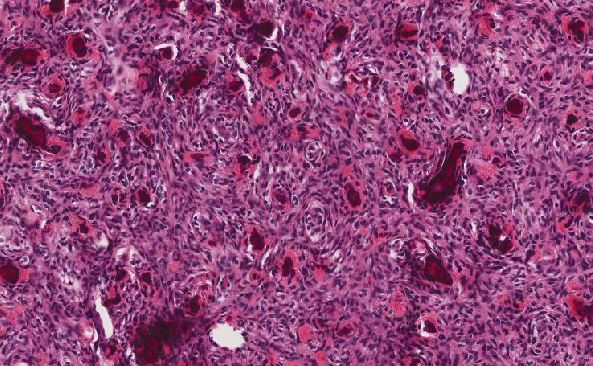
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May