Residency Program - Case of the Month
June 2012 - Presented by Rebecca Sonu, M.D.
Answer:
Ovary: Mixed epithelial carcinoma; Appendix: Goblet cell carcinoid
Histological description:
Ovary
Microscopically, sections of the ovarian tumor showed three different histological types: mucinous (75%), clear cell (15%) and serous (10%). The mucinous component of the tumor showed cysts and glands lined by columnar epithelial cells containing intracytoplasmic mucin (Figure 1). The serous papillary component showed irregular, complex branching and cellular papillae lined by stratified cuboidal to columnar epithelial cells. Orderly penetration of the stroma by glands without stromal reaction were seen (Figure 2). The clear cell component showed a few clusters of solid nests composed of clear cells. Hobnail cells lined the lumens and papillae. The clear cells are rounded or polyhedral, have distinct cell borders and contain eccentrically rounded nuclei with prominent nucleoli. The hobnail cells contain bulbous dark nuclei that protrude into lumens (Figure 3). Notice the dense hyaline basement membrane material expanding the cores of the papillae.
Appendix
Microscopically, sections of the tip of the appendix showed a thickened and fibrotic wall (Figure 4) with small uniform nests of goblet cells arranged in a microglandular fashion infiltrating through the muscularis propria, into the subserosa and to the serosal surface (Figure 5-9). A desmoplastic response surrounds the tumor nests within a fibromyxoid background. On higher-power the tumor nests are composed of a single layer of goblet cells that are round with basally oriented dark nuclei. The cytoplasm is filled with light-purple mucin. Lymphovascular space invasion was identified. The uninvolved portion of the appendix shows a submucosal lymphoid aggregate (Figure 10). The tumor cells stained positive for chromagranin (Figure 11), positive for carcinoembryonic antigen (CEA) (Figure 12), positive for cytokeratin (CK) 20 (Figure 13), and positive for Mucicarmine (MUC) 2 (Figure 14).
Discussion:
Mixed epithelial ovarian carcinomas represent less than 4% of epithelial-stromal tumors and consist of two or more histologic types within the same tumor. The five major histologic categories include: serous, mucinous, endometrioid, clear cell and transitional.1 According to the World Health Organization (WHO) convention, mixed epithelial ovarian tumors are those in which the minor components are grossly recognizable, or account for at least 10% of the tumor on microscopic examination. Therefore, sampling of the tumor should be extensive enough to include all the different components.2 Due to the grossly and microscopically recognizable mucinous component at frozen section analysis, staging including appendectomy was performed.
Most ovarian mucinous cystic tumors associated with pseudomyxoma peritonei are metastasis as almost all are appendiceal origin.1 Although mucinous ovarian tumors are currently classified as surface epithelial tumors, their origin is unclear in most cases. Therefore, it was important in this case to determine whether the ovarian mass originated from the appendix even though it was of mixed-epithelial type. It was also a convenient time to perform the appendectomy.
The goblet cell carcinoid found in the appendix was determined to be an incidental finding and unrelated to the ovarian mass. Based on morphology, the goblet cell carcinoid cells were markedly different than the cells of the mucinous component of the ovarian mass (see microscopic description above). In addition, the immunohistochemical staining confirmed that these two pathologies were separate (see next paragraph and Table).
Goblet cell carcinoid is one of the major types of appendiceal tumors traditionally included in the neuroendocrine category. It has also been called ‘goblet cell type adenocarcinoid’, ‘mucinous carcinoid tumor’, ‘microglandular carcinoma’, and ‘crypt cell carcinoma’. GCCs present in the fifth to sixth decade and show no definite sex predominance. The most common clinical presentation is acute appendicitis, followed by abdominal pain and a mass. Fifty percent of the female patients present with ovarian metastases.3 Goblet cell carcinoid is derived from the mucosal pluripotent crypt cells in mucosal crypt epithelia. Grossly, it may be found in any portion of the appendix. Mucicarmine and CEA stains are consistently positive. CK20 is present in all cases and CK7 in about 70% in a focal fashion. CK18 and CD99 are frequently expressed. It is important to know that this goblet cell tumor is much more aggressive than the classic carcinoid, particularly if the tumor shows transmural involvement, such as in this case.4
The differential diagnosis should include the classic (insular) carcinoid tumor, which can be distinguished by the typical solid nests of small monotonous cells with occasional acinar or rosette formation. The large majority of these tumors are argentaffin; argyrophilic filled. IHC will stain positive for NSE, Chromogranin, and synaptophysin. This tumor can be distinguished from goblet cell tumor with CK20; CK20 is usually positive in classic carcinoid but should be negative for mucicarmine.
Goblet cell carcinoid may also be combined with either a signet ring cell type adenocarcinoma or a poorly differentiated adenocarcinoma.5 A combined GCC with classic carcinoid has been proposed as a new morphologic variant of carcinoid tumor.6 It was questioned whether this tumor is a “collision” or “hybrid” type of tumor. Chetty et a.l and Khor et al. favor it as being a “hybrid” tumor originating from a presumptive common precursor with the capacity for diverent differentiation.6,7
References:
-
SJ Robboy, GL Mutter, J Prat, RC Bentley, P Russell, MC Anderson, eds. Robboy’s Pathology of the Female Reproductive Tract. 2nd Ed. Churchill Livingstone, 2009.
-
Scully R, Sobin LH. World Health Organization (WHO) Histological Typing of Ovarian Tumours. 2nd Ed. World Health Organization. International Histological Classification of Tumours.
-
Chetty R, Roy P. Goblet cell carcinoid tumors of the appendix: An overview. World J Gastrointest Oncol. 2010;2(6):251-8.
-
Rosai J. Rosai and Ackerman’s Surgical Pathology. 10th Ed. Philadelphia, 2011.
-
Tang LH, Shia J, Soslow RA, et al. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol. 2008;32:1429-1443.
-
Chetty R, Klimstra DA, Henson DE, et al. Combined classical carcinoid and goblet cell carcinoid tumor: A new morphologic variant of carcinoid tumor of the appendix. Am J Surg Pathol. 2010;34:1163-1167.
-
Khor TS, Shen J, Lauwers GY, et al. Letter to the Editor: Comment on the article by Chetty et al on Combined Classical Carcinoid and Goblet Cell Carcinoid Tumor: A new morphologic variant of carcinoid tumor of the appendix. Am J Surg Pathol. 2010;35(8):1248-1250.

 Meet our Residency Program Director
Meet our Residency Program Director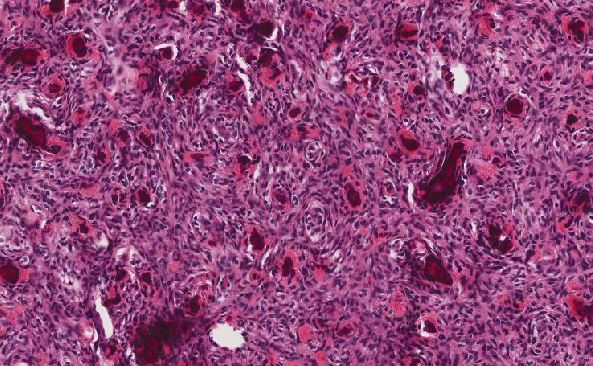
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May