Residency Program - Case of the Month
June 2011 - Presented by Meighan Tomic, M.D.
Answer:
Hepatic Epithelioid Hemangioendothelioma
Histological description
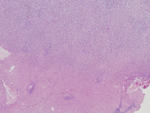
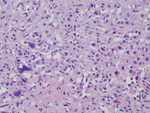
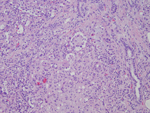
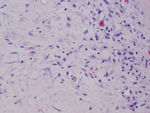
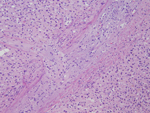
Sections of the tumor showed a vascular neoplasm with infiltrative borders. The neoplastic cells were present in nodules and large sheets with alternating hypercellular and hypocellular areas. The tumor filled the hepatic lobules with preservation of the portal tracts. In some areas, the tumor entrapped single hepatocytes and cords of hepatocytes. The neoplastic cells varied from epithelioid to spindled. The epithelioid cells were intermediate to large in size with pink to amphopillic, finely vacuolated cytoplasm with ill-defined cells borders. Occasional multi-nucleated cells and cells with intracytoplasmic lumens were present. The nuclei were ovoid to round with coarse chromatin. Some nuclei were hyperchromatic and had irregular contours and prominent nucleoli. The hypocellular areas showed spindled and stellate cells in a myxohyaline stroma. Intravascular polypoid projections of epithelioid cells were present, and tumor was also present filling large veins. Necrosis and mitoses were absent. The neoplastic cells stained with CD31, factor VIII, and factor XIIIa.
Discussion:
Epithelioid hemangioendothelioma (EHE) is a rare vascular neoplasm that has been described in soft tissue, liver, lung, bone, skin, lymph nodes, peritoneum, brain and meninges (1). The pathogenesis of this tumor is not well understood and risk factors have not been identified (1).
In the liver, the differential diagnosis for this tumor includes carcinomas (cholangiocarcinoma and metastatic signet ring cell carcinoma) and other vascular neoplasms (angiosarcoma). Recognition of vascular proliferation helps differentiate EHE from carcinoma. Staining of the neoplastic cells with endothelial cell markers (FVIII, CD34, CD31) and lack of staining for mucin, bile, CEA or AFP confirm the diagnosis. The dense sclerosis and hyalinization frequently present in EHE help distinguish it from angiosarcoma. EHE also has a more solid appearance while angiosarcoma is more vascular. Further, angiosarcoma is characterized by the hobnail appearance of hyperchromatic malignant endothelial cells protruding into vascular spaces. Finally, angiosarcoma typically displays more marked atypia and more frequent mitoses and necrosis.
The largest series of hepatic epithelioid hemangioendotheliomas consisted of 137 cases (1966-1997) from the files of the Armed Forces Institute of Pathology (2). The mean age of the patients in this series was 47 years and the female to male ratio was 1.6:1 (2). The presenting symptoms were upper abdominal pain and weight loss in 45% of cases, however 22% of cases were asymptomatic (2). Elevated alkaline phosphatase was the most common laboratory abnormality (present in 75% of patients at presentation) (2). The most common abdominal CT findings were multiple hypodense lesions with a hyperdense periphery after contrast administration (2).
On gross examination, the majority of patients had multiple lesions (82%). The tumors ranged in size from 0.2 to 14 cm and the majority had firm to rubbery, pale to white cut surfaces (2). Microscopic exam revealed infiltrative vascular neoplasms comprised of spindled to epithelioid cells (2). The tumors had hypercellular and hypocellular areas, and the stroma varied from spare fibrillar to hyaline stroma to plentiful sclerotic to myxohyaline stroma (2). Infiltration of sinusoids, terminal hepatic venules, and portal vein branches was common (2). Intravenous polypoid projections of epithelioid cells were present in 78% of cases (2). The epithelioid cells varied from intermediate to large in size and had eosinophillic cytoplasm and vesicular nuclei with inconspicuous nucleoli (2). Multinucleated cells were present in 29.2% of cases (2). Moderate nuclear atypia was present in half of the cases and severe atypia was present in a quarter (2). The majority of cases (58%) had no mitoses; 9% of cases had 2-4/10HPF and 4% had 5-8 mitoses/10HPF (2). Please see Table 1 for a summary of the immunohistochemical staining results.
The behavior of epithelioid hemangioendothelioma is unpredictable (1). In this series follow up data was available for 60 patients. Survival ranged from 4 months to 28 years (2). Forty three percent of patients survived greater than or equal to five years, but an equal percentage died within 4 to 16 months (2). High cellularity was the only histopathologic feature that significantly correlated with poor clinical outcome (reduced overall survival) (2). The definitive treatment for hepatic epithelioid hemangioendothelioma is surgical resection. However, given the multifocal nature of this tumor resection is not always possible. In such cases liver transplant may be considered.
Table 1: Results of Immunohistochemical Staining
| Quantization of staining | |||||
| Antibody | No. of cases | % positive | <25% | 25-75% | >75% |
| FVIII-RAg | 131 | 99 | 13 | 32 | 55 |
| CD34 | 70 | 94 | 13 | 36 | 36 |
| CD31 | 66 | 86 | 49 | 39 | 12 |
| FXIIIa | 6 | 100 | 66 | 0 | 33 |
| Vimentin | 68 | 93 | 22 | 33 | 45 |
| Type IV collagen | 50 | 94 | |||
| Laminin | 50 | 88 | |||
| Smooth muscle actin | 57 | 26 | |||
| Cytokeratin | 63 | 14 | |||
Taken from Makhlouf et al. Cancer 1999.
References:
- Weiss SW, Goldblum JR. Hemangioendothelioma: vascular tumors of intermediate malignancy. In: Soft Tissue Tumors Fifth Edition. Philadelphia: Elsevier, 2008.
- Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemagioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 1999;85:562-582.

 Meet our Residency Program Director
Meet our Residency Program Director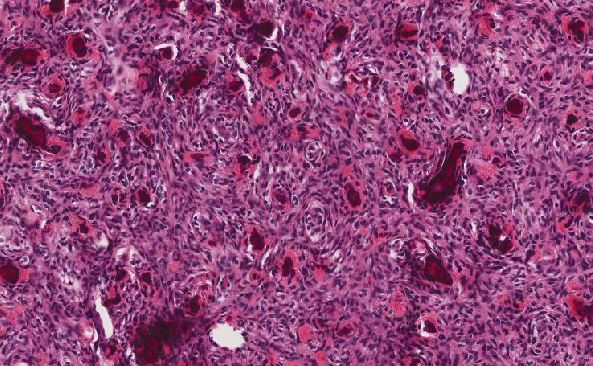
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May